It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Modified Work-Task Assignments and Return to Work Status for the Injured Employee: Suggestions for the Provider
For health care providers, the necessity of a modified work-task assignment and/or return to work status can sometimes be difficult to ascertain. However, the provider can utilize the facts discovered during the history and examination to make this challenging determination a much easier task. One goal of every practitioner is to return the employee to work as quickly as possible. However, the highest regard for the employee's safety and prevention of further injury while at work remains a primary concern. To allow the employee to return to work, the provider must obtain a mental picture of the employee's task and activity habits while questioning the employee about the exact nature of the illness or injury.
To obtain the necessary background information, the provider's history and chief complaint consultation may include the following or similar questions [see Figure 1]: Has the employee described exactly what she/he was doing when injured? What is the employee's job description? (Give details.) What are the job task activities that are required to do the work? What does the employer require the employee to do to complete the task(s)? Have there been any recent changes of equipment and tools used or other modifications of the workstation? How many hours/day does the employee perform the task(s)? However, for further clarification, the provider may ask additional questions such as if the employee has more than one task that encompasses the work-time, and if so, the activities of the various tasks. From a more descriptive history, the practitioner should be able to better determine the exact mechanism of injury to formulate a hypothesis for a modified work-task assignment or the most appropriate time to return to work.
Symptoms of pain are usually the chief factors in causing an employee to seek chiropractic/medical care. These symptoms may result from either of two major classes of injuries: acute and repetitive strain injuries (RSI) and cumulative trauma disorders (CTD). Each class has its own intricacies that must be resolved before the employee can return to work. For acute injuries, the mechanism of injury involved should be determined so that other possible complicating conditions may be determined. These complicating conditions may be in two areas.
- Minor areas of injury distant to the site of complaint, such as a soft tissue condition in the form of a sprain/strain injury to the neck received as a result of a fall that precipitated the primary injury in the lower back or a lower extremity.
- Underlying conditions that may affect the biomechanics of the area involved, such as scoliosis, degenerative joint disease, congenital, surgical fusions, scar tissue, occupational illnesses, etc. (see Figure 2).

When there are acute exacerbations to occupational illnesses (RSIs and CTDs), the necessity of modification of the task activities and work assignments is greatly enhanced. If the work habits have contributed to the advancement of the condition, further retraining is recommended to avoid habitual or static postures and movements that will tend to act in synergy with the condition or retard the healing progress. If the common tools used during the course of the work day are contributory, then ergonomically designed equipment would be most beneficial to help reduce or prevent reinjury.
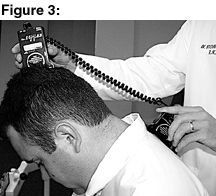
To obtain a detailed, comprehensive objective orthopedic examination, precise range of motion (ROM) studies of the involved area(s) must be determined by using accurate recording devices such as inclinometers or computerized ROM and joint testing equipment (see Figures 3-4). Neurological testing is vital to accurately determine if there is any loss of proprioception or tactile/sensory perception that would preclude the employee from performing useful duties. Also, an appropriate, standardized muscle testing system is recommended to measure muscle strength against gravity and the resistance applied by the examiner. The AMA guidelines for impairment ratings can be a reliable source to obtain the specific rules for testing ROM and for grading muscle strengths to the involved area(s).
Almost all providers conduct similar testing on a daily basis. However, the type of testing that is done in the provider's office is usually more clinical in nature and may not be comprehensive enough for the case presented, or be able to be accurately measured by using proper instrumentation. Often there is no plan or need to follow up with a patient as to ascertain temporary disability. Therefore, the results are not usually correlated and tabulated for convenience or ease of interpretation. An accurate estimate of temporary disability is not possible without the forethought to use proper procedures.

To determine if the employee is able to return to work or requires modifications to their normal work activities, the provider must make a determination of the approximate level of temporary/permanent impairment. The impairment is derived from the examination data. The impairment can then be converted to an accurate temporary disability for certain activities. This temporary disability for a specific activity can then be compared to the chief activities performed by the employee to determine if the disability precludes the employee from performing the activities in the performance of assigned job tasks.
This is how the temporary disability determination might be done. Employee A and employee B work for a small shipping firm. Both weigh 195 lbs. and are 5'10". Neither employee belongs to a gym or works out regularly. Employee A works in the accounting office. Employee B works in the warehouse.
While doing inventory of supplies in the warehouse, Employee A moves a box (see figure 5), steps backward, pushes on the box, and feels a sudden stabbing pain in the lower back. Employee B, while stacking boxes on a wooden pallet, feels a stabbing pain in the lower back. Both employees have been examined and do not show indication of acute intervertebral disc involvement. There is no indication of complete muscle tear in either case. There are no gross significant findings on the radiological exam.
The diagnosis is mild lower back strain for each employee. Therefore, a detailed, descriptive history of the employee's mechanism of injury, work environment and job task activities are necessary to determine if the employee should have modification to the workstation or job duties.
As stated previously, employee A is an office worker in the accounting department, rarely enters the warehouse and does not bend and lift; the regular job classification is sedentary. During the acute phase of treatment, this employee should be released from work for a duration of four days.1 While employee A might be uncomfortable and need aggressive treatment after the four days, the employee should return to regular duty with the exception of bending, stooping, and lifting, all of which are not normally a part of the employee's job description.
Employee B is a regular warehouse worker and must bend, twist and lift regularly. During the acute phase of treatment, this employee should be released from work four days.1 However, in addition, this employee must have an alteration of job description to return to work. While the short-term healing time in this case is about three weeks, the healed torn muscle tissue retains only about 15% of its normal strength,2 so an additional six weeks to six months may be required to complete the healing process.
When only mild strain is involved, the doctor should recommend universal precautions such as back supports, rest periods, and ergonomically designed tools such as hoists and lifts. Employee cross-training is also recommended to reduce the activity which caused the original injury.
According to Mazion, each employee's job task is composed of various activities, such as standing, sitting, stooping, bending, carrying and lifting.3 In the case of employee B, the recommendation would be to temporarily (six weeks) decrease or eliminate lifting, bending and stooping due to the possibility of reinjury.
This alteration in activity could be accomplished in various ways, such as having an assistant help share the burdens of lifting, and heightening the pallets and articles to waist level so that no bending or lifting is needed (for clarification, lifting involves changing the level of the object, while carrying does not). When it becomes necessary for an employee to stoop, as in reading labels at waist level or lower, a low rolling stool could be used to position the employee closer to the work environment at hand, which helps to reduce or eliminate the straining stance [see Figure 6].
In summary, these examples or ideas may seem very simplistic in nature and might be regarded as common sense by many providers. Often these examples are simply overlooked, and the provider simply makes an educated guess to restrict the employee's activities. If the provider converts each job task into the various physical activities required for the performance of the task, then he/she should be able to restrict duties in a logical manner and make recommendations for alteration of the task or tools used to complete the task. This could possibly reduce the risk of reinjury and increase productivity with feelings of well being by the employee.
Acknowledgements:
The authors wish to thank John Coats, DC, for his assistance with the sensory test, and interns Charles O'Neil, Mark Benton and Nathan Unruh for their assistance with the illustrations.
References
- Official Disability GuidelinesTM: Length of Disability Data by ICD-9-CM from CDC and OSHA Plus NHDS Hospital Length of Stay. Connecticut: Work-Loss Data Institute, LLC, 1996.
- Foreman S, Croft AC. Whiplash Injuries: The Cervical Acceleration/Deceleration Syndrome. Maryland: Williams & Wilkins, 1995, pg. 338.
- Mazion JM. Applied Spinal Disability Evaluation. Arizona: Mazion, 1985.



