It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
The State of the Art - "Evidence-Based Care": Part Three of a Four-Part Series
Introduction
Diagnosis of structural pathology does not adequately guide treatment decision-making. Disc bulges are present in 52% of asymptomatics.1 Surprisingly, the larger the disc herniation the more likely nerve root compression is to spontaneously resolve.2 If diagnosis of structural pathology does not consistently correlate with symptoms, what evaluation can guide our treatment decisions? Evaluation of dysfunction is essential for figuring out what is causing pain in the locomotor system. This is called the "sports medicine approach." Its main emphasis is in identifying and treating the deconditioning syndrome (see Table 1). Athletes know that functional restoration is the key to return to competition, and that diagnosis of tissue injury or pathology is only a starting point.
Table 1: The Deconditioning Syndrome
- physical
- decreased endurance of deep stabilizers
- motor control dysfunction
- psychological
- abnormal illness behavior
Disabled workers are now viewed as occupational athletes. Repetitive tasks stress the locomotor system beyond what it can handle. Deconditioning must be addressed, and reactivation is a key to recovery. In the recent occupational health guidelines from England, a functional approach is considered essential.3 Maintenance of activities is encouraged even if there is still some back pain. Specific advice on activity modifications is strongly recommended. If a patient expects passive treatment and doesn't believe that active participation will help, it correlates with a slower recovery. The guidelines urge practitioners to address the common misconception that patients need to be pain-free to resume activities.
Table 2: The Kinetic Chain Approach
- History: Identify the clinical symptom complex.
- Examination:
- Identify the tissue injury complex.
- Identify the source of biomechanical overload.
- Identify the dysfunctional kinetic chain.
To avoid the trap of limiting treatment to the site of symptoms or pathology the "kinetic chain approach" is recommended by Kibler et al. (see Table 2).4
As an example, think of a patient with a rotator cuff syndrome. The typical presenting clinical symptom complex is anterolateral shoulder pain. The tissue injury complex is often rotator cuff tendinosis. Usually, orthopedic treatment is of the injured tissues or inflammation (medication, physical therapy modalities, injection, surgery). However, unless the source of the biomechanical overload is identified, relapse or recurrence is inevitable. In this example, there is likely to be subacromial impingement, which must be addressed. The dysfunctional kinetic chain may involve a stiff posterior shoulder capsule, weak lower scapular fixators, tightness in the pectorals and upper trapezius, and an altered scapulohumeral rhythm. If treatment is limited to the painful or injured area, and if key dysfunctions in the kinetic chain are not addressed, symptom recurrence or reinjury is likely.
Table 3: Components of the Spine Stability System
- central nervous subsystem (control)
- steoligamentous subsystem (passive)
- muscle subsystem (active)
Mechanism of Injury of the Spine
Injury occurs when external load exceeds the failure tolerance or strength of the tissue. Injury covers a broad spectrum from simple irritation to fracture, avulsion or rupture. Most low back injuries are not the result of a single exposure to a high magnitude load, but instead a cumulative trauma from sub-failure-magnitude loads. For instance, repeated small loads (e.g. bending) or a sustained load (e.g. sitting). In particular, low back injury has been shown to result from repetitive motion at end range. According to McGill, it is usually a result of "a history of excessive loading which gradually, but progressively, reduces the tissue failure tolerance."5
What protects the spine? Devoid of its musculature, the spinal column has been found to buckle at a load of 20 newtons at L5, yet during normal motions, the spine handles loads 20 times that on a routine basis. Panjabi has concluded: "This large load-carrying capacity is achieved by the participation of well-coordinated muscles surrounding the spinal column."6 According to Panjabi, the following subsystems work together to promote stability (see Table 3).
Stability is due to passive ligament stiffness and active muscle stiffness, which prevent excessive end-range loading knowing when and how these passive and active components become dysfunctional is essential to guide injury prevention advice and programs. After only 20 minutes of sitting, creep occurs in the posterior ligaments, which compromises stiffness for some time, even after changing posture.6a Surprisingly, the combination of prolonged end-range loading and low load is a common mechanism of spine injury. Every back pain specialist realizes that most low back injuries occur under situations of very low (or even trivial) load. It is now possible to explain the biomechanics of this injury mechanism.
Normally, spinal muscles are automatically highly active under conditions of appreciable load. Cholewicki and McGill have shown how under relatively low load conditions, a motor control error - for instance, an error due to fatigue - can temporarily reduce activation of deep intersegmental muscles (i.e.) required for preventing end range loading.6b A typical example of this would be when an individual sits for a prolonged period of time, thus encountering both end-range loading and fatigue of ligaments that normally provide passive restraint or stiffness to the spine. The individual then bends forward for a pencil on the floor and experiences immediate, acute low back pain (LBP). Load is low, thus muscle activation is low. Since passive stiffness was already compromised, low back injury with trivial load results.
Interestingly, it is not strength but coordination between agonist and synergist muscles which plays a pivotal role in resisting injury. Sparto et al., reported that spinal loading forces were increased during a fatiguing isometric trunk extension effort without a loss of torque output.7 Torque output remained constant because as the erector spinae fatigued, substitution by secondary extensors such as the internal oblique and latissmus dorsi muscles occured.
Radebold et al., showed that back pain patients have a different muscle response pattern in response to load handling.8 Patients had slower reaction times than controls and increased co-activation patterns. Wilder et al., has also shown slow reaction time, decreased peak output, and increased after discharges when irregular load is handled.9
Specific dysfunction of the transverse abdominus and multifidus has also been shown in back pain patients. Hodges and Richardson showed that delayed activation of transverse abdominus during arm movements distinguishes LBP patients from normals.10,11
Similarly, a decreased activation of the transverse abdominus/oblique abdominals (IO/TA) relative to the rectus abdominus (RA) was correlated with LBP.12 Control subjects were able to preferentially activate IO/TA without significant RA activiation whereas LBP patients could not do this.
Decreased endurance of the trunk extensors has not only been shown to correlate with pain, but to predict recurrences and first time onset in healthy individuals.13,14 This evidence is extremely strong because it is prospective. The multifidus in the low back has been shown to be atrophied in patients with acute low back pain.15 The acute patients' atrophy was unilateral to the pain and at the same segmental level as palpable joint dysfunction. Recovery from acute pain did not automatically result in restoration of the normal girth of the muscle.16 However, spinal stabilization exercises successfully rebuilt the muscle's size. Recent research demonstrates that individuals who successfully restore normal multifidus girth have fewer recurrences at both one and two-year follow-up.17
Biomechanical Aspects of Reactivation
Muscles can work to either produce or control movement. Traditionally, emphasis has always been placed on movement production, but injury prevention depends more on movement control than strength. Bergmark was the first to describe two distinct muscle systems: one functioning to produce movement, the other to control it.18 Superficial muscles are responsible for producing voluntary movement or generating torque, while deep muscles are responsible for maintaining joint stability. The deep ("intrinsic") muscles are responsible for joint stability on an involuntary or subcortical basis.
What are the 1-degree stabilizers of the spine? The deep-local muscles are primarily responsible for joint stability. These are shorter, "intrinsic" muscles with fewer attachments. They are close to the joint's center of rotation (e.g. multifidus & transverse abdominus) in contrast to superficial-global muscles that span many segments or multiple joints (e.g.,erector spinae & rectus abdominus).
Surprisingly, the one muscle highly active during flexion, extension and lateral bending tasks is the quadratus lumborum.19 Its architecture is ideally suited to be a stabilizer since it attaches each transverse process to the more rigid pelvis and rib cage, facilitating a bilateral buttressing effect for the vertebrae.20
Axler and McGill have demonstrated that muscle output and spinal load can be measured for a variety of exercises.21 Muscle output is determined as a percentage of maximum voluntary contraction ability (MVC) and spinal load as a measure of spinal compression and shear forces. Ideal exercises are those with a high ratio of muscle challenge to spinal load. Such analyses give surprising data about common exercises that are prescribed for low back pain. For instance, spinal load is not different during sit-ups with knees bent or straight. In either case, the load is over 3000N and therefore should not be prescribed in the low-back-recovering population!21,22 There are safer back exercises.
Safe back principles have emerged from rigorous analyses of biomechanical and kinesiological aspects of spinal function.23-28 By emphasizing endurance training of key spinal stabilizers, positive outcomes have been achieved.12,17,29 These principles can be summarized into a user-friendly approach that will enhance clinical application and patient compliance.
The main emphasis of rehabilitative exercise is to train "inner range" or core muscle endurance. This requires kinaesthetic awareness of "neutral spine" postures and regular sustained training of this motor control against a variety of challenges. Multiple reps of 5-6 "s-holds" daily should be performed. According to Manniche et al., up to three months may be required to achieve a long-lasting beneficial effect.30
Ideal exercises will challenge muscles, impose minimal joint load to spare the spine, and train joint stability in a "neutral posture" w/ agonist-antagonist coactivation. Exercises are performed in the patient's "functional range." According to Morgan, this is "the most asymptomatic and stable position or range for the task at hand."31
Why is this unique intersegmental stabilization approach needed? Exercise programs which focus only on strengthening and ignore coordination may inadvertently reinforce substitution patterns by encouraging "trick" movements. Grabiner showed that resistance exercises for trunk extension can be performed with symmetry or asymmetry of extensor musculature.32 Symmetry is characteristic of non-injured back patients whereas asymmetry is typical of the back-injured population. Muscle imbalance consisting of underactivity of agonists and overactivity of synergists was able to discriminate whiplash pain patients from asymptomatics with 88% accuracy.33 Strength was not less in the injured group due to synergist substitution. Sparto et al., showed that spinal load increases during a fatiguing isometric trunk extension effort without a loss of torque output because of synergist substitution.7 Finally, overactivation of the rectus abdominus along with underactivity of the IO/TA has been correlated with LBP.12
Table 4: Active Care
Level One - Advice
- the dangers of deconditioning & value of incremental re-activation
- activity modifications during activities of daily living (ADL) such as sitting & lifting
- how to co-activate muscles capable of "bracing" the spine in a "neutral posture"
- how to tell the difference between hurt & harm
Level Two - Exercise
- Endurance training deep muscles is responsible for joint stability
- Control of movement is more important than strength or speed of movement
Active Care Principles
Active care addresses both the psychosocial and biomechanical features of back problems. It consists of two basic levels: reactivation advice and motor control exercise (see Table 4).
Table 5: The 360-Degree Approach
- Train postural control (i.e. position sense) of the back's "neutral position."
- Train endurance of the muscles which can maintain "neutral" in all 360 degrees (anteriorly, laterally and post.)
- Troubleshooting
- Flexibility for peripheral muscles & joints - ankle, knee & hip
- Progressions
- Keep exercises reasonably difficult (Borg Scale of Exertion).34
- Increase stability challenge by using labile surfaces (gym balls, rocker boards).
- functional whole body activities (squats, lunges)
In our report of findings, on day one, patients receive education that explains why active care is important to recovery; how the "deep" muscles are responsible for joint stability; the importance of performing movements within one's "functional range" so as to promote healing and avoid reinjury; and that activity advice will be simple and concise with regular adjustment so the home program can be customized. Self-treatment advice will be linked to activities of daily living (ADLs) and functional goals.
Prescribing exercises for the back-injured patient follows a systematic approach. This is called the "360-degree approach" (see Table 5)
A patient with a chief complaint of low back pain may receive a diagnosis of facet syndrome, but this is insufficient to guide treatment. The source of biomechanical overload may be end-range spinal loading in extension due to poor activation of the deep abdominal muscles. In such a case, treatment of the pain-generating facet joints by adjustment may only yield short-term relief. Stabilization may require training the kinaesthetic awareness of how to activate the deep abdominal muscles, such as transverse abdominus, to "brace" the lumbar spine in a "neutral range." Additionally, such end-range overload in lumbar extension may also be perpetuated by stiffness in peripheral joints such as the hip in extension. A common kinetic chain dysfunction called the "lower-crossed" syndrome involves decreased hip extension mobility and compensatory increased lumbo-sacral hyperextension strain.35 Thus, along with adjustment of the pain-generating lumbar facet join, and facilitation of the inhibited transverse facilitation of the inhibited transverse abdominus muscle, release and lengthening of the hip flexor muscles (i.e. psoas) may be necessary to stabilize the kinetic chain.
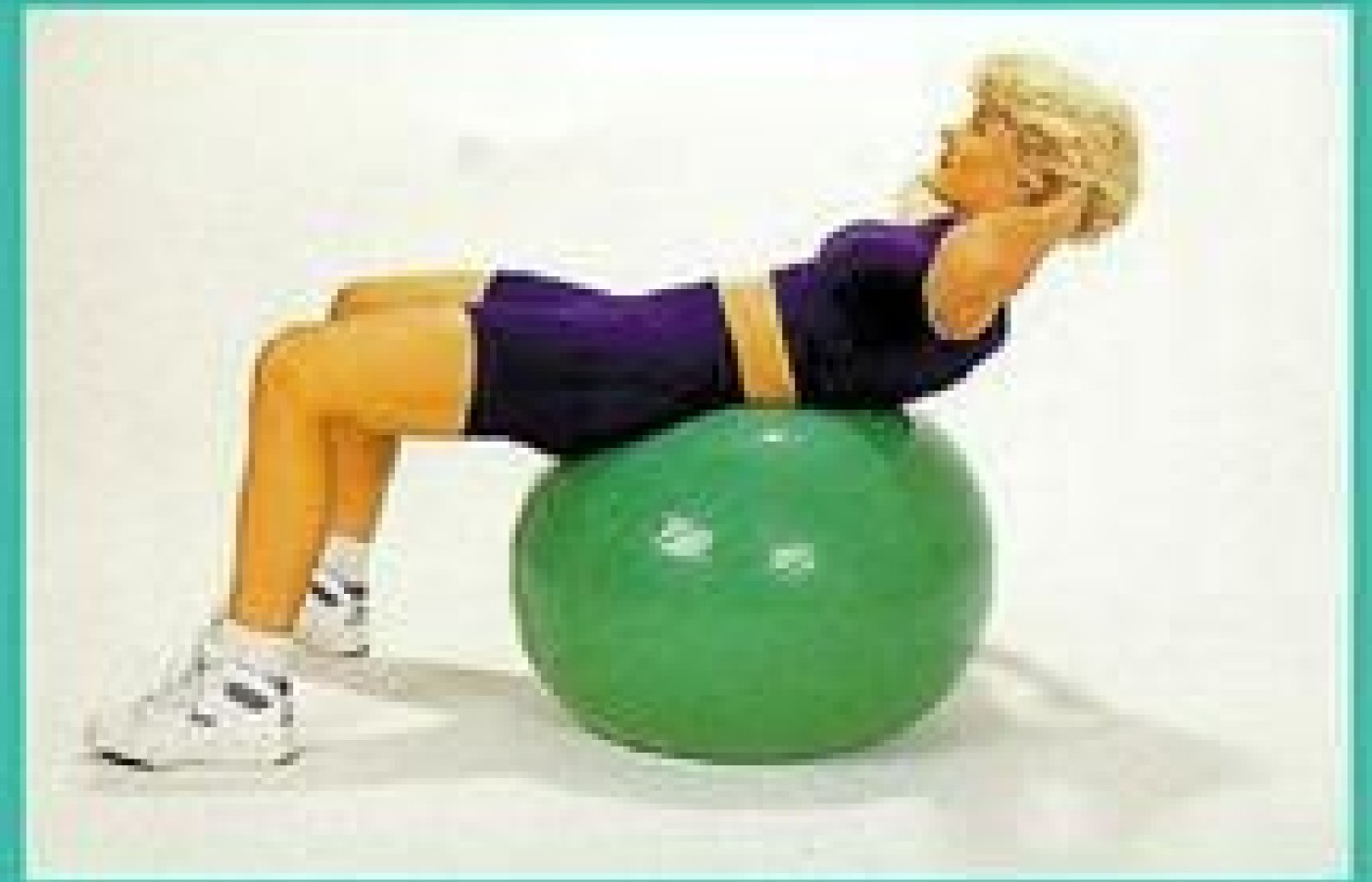
The core principles of active care are easily applicable in a neuromusculoskeletal practice. They consist of isolation of the "deep" muscles and avoidance of substitution patterns.10-12 Once proper form is demonstrated, endurance training of key stabilizers is commenced.5,12,23 Progressions involving the use of labile surfaces such as gymnastic balls have been shown to increase stabilization muscle activity 400% over floor exercises, without a significant increase in spinal load (see Figure 1).36
Figure 1

Trunk curl-up on a gymnastic ball
Active care is simple to integrate into chiropractic practice. This article has presented the biomechanical foundation for exercise and its place in the overall improvement of function throughout the kinetic chain. Deconditioning is both physical and psychological, so functional reactivation treatment must follow both psychosocial and biomechanical principles. The first level of active care is simple advice that reassures patients regarding the benefits and safety of early reactivation. The main purpose is to promote healing and prevent deconditioning. The second level involves endurance and motor control training designed to enhance joint stability.
The final paper in this four-part series on evidence-based spinal health care will review the "tools of the trade" for utilization of active care in neuromusculoskeletal practice. Typical perceptions that interfere with the chiropractic adoption of evidence-based active care methods for pain in the locomotor system will be addressed. These include myths that exercise is harmful; takes too much time; and requires expensive equipment, costly staff or additional space. The one idea, that should probably be clear as a result of this series is that active care is essential for "benchmarking" chiropractors as experts in managing disorders of the locomotor system.
Acknowledgement: The author would like to thank Stuart McGill for his tireless investigations into the mechanisms and treatment of spine instability.
References:
1. Jensel MC, Brant-Zawadzik MN, et al. N Engl J Med 2:69, 1994.
2. Bush K, Cowan N, Katz DE. The natural history of sciatica. Spine 1992;17:205.
3. Waddell G, Burton AK, 2000. Occupational health guidelines for the management of low back pain at work - evidence review. Faculty of Occupational Medicine. London.
4. Kibler WB, Herring SA, Press JM. Functional Rehabilitation of Sports and Musculoskeletal Injuries. Aspen, 1988.
5. McGill SM 1998. Low back exercises: prescription for the healthy back and when recovering from injury. In: Resources Manual for Guidelines for Exercise Testing and Prescription. 3rd ed. Indianapolis, Ind: American College of Sports Medicine. Baltimore, Williams and Wilkins.
6. Panjabi MM. The stabilizing system of the spine. Part 1. Function, dysfunction, adaptation, and enhancement. J Spinal Disorders 1992;5:383-389.
6a. McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clin Biomech 1992;7:43-46.
6b. Cholewicki J, McGill S M 1996 Mechanical stability of the in vivo lumbar spine: Implications for injury and low back pain. Clin Biomech 11:1-15.
7. Sparto PJ, Paarnianpour M, Massa WS, Granata KP, Reinsel TE, Simon S 1997. Neuromuscular trunk performance and spinal loading during a fatiguing isometric trunk extension with varying torque requirements. Spine;10:145-156.
8. Radebold A, Cholewicki J, Panjabi MM, Patel TC. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine 2000;25:947-954.
9. Wilder DG, Aleksiev AR, Magnusson ML, Poper MH, et al. Muscular response to sudden load. Spine 1996;21 (22):2628-2639.
10. Hodges PW, Richardson CA 1996. Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine 21:2640-2650.
11. Hodges PW, Richardson CA 1998 Delayed postural contraction of the transverse abdominus associated with movement of the lower limb in people with low back pain. J Spinal Disord 11:46-56.
12. O'Sullivan P, Twomey L, Allison G 1997. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolysthesis. Spine 24:2959-2967.
13. Biering-Sorensen F 1984. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 9:106-119.
14. Luuto S, Heliovaara M, Hurri H, Alaranta H 1995. Static back endurance and the risk of low-back pain. Clin Biomech 10:323-324.
15. Hides JA, Stokes MJ, Saide M, Jull Ga, Cooper DH 1993. Evidence of lumbar multifidus muscle-wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine 19(2):165-172
16. Hides JA, Richardson CA, Jull GA 1996a. Multifidus muscle recovery is not automatic after resolution of acute, first-episode of low back pain. Spine;21(23):2763-2769.
17. Hides JA, Richardson CA, Jull GA 1996b. Mulitifidus muscle rehabilitation decreases recurrence of symptoms following first episode of low back pain. In: Proceedings of the National Congress of the Australian Physiotherapy Association, Brisbane.
18. Bergmark A 1989. Stability of the Lumbar Spine. Acta Orth Scand Supp 230(60);20-24.
19. McGill SM, Juker D, Kropf P 1996;.Quantitative intramuscular myolectric activity of the quadratus lumborum during a wide variety of tasks. Clin Biomechanics 11(3);170-2.
20. McGill SM sched pub 2000.. Clinical biomechanics of the thoracolumbar spine in Clinical Biomechanics (ed Dvir Z), in press.
21. Axler CT, McGill SM 1987. Low back loads over a variety of abdominal exercises: searching for the safest abdominal challenge. Med Sci Sports Exerc. 29:804-810.
22. McGill S 1995. The mechanics of torso flexion: situps and standing dynamic flexion maneuvers. Clin Biomech 10:184-192.
23. McGill SM 1998.Low back exercise: evidence for improving exercise regimens. Phys Ther 78:754-765.
24. Liebenson CS 1999. The safe back workout. JNMS,7(1).
25. Lewit K. Manipulative Therapy in Rehabilitation of the Motor System. 3rd edition. London: Butterworths, 1999.
26. Liebenson C. Rehabilitation of the Spine: A Practitioner's Manual, Liebenson C (ed). Williams and Wilkins, Baltimore, 1996.
27. Liebenson C, Chapman S. Rehabilitation of the Spine: Functional Evaluation of the Lumbar Spine, Williams & Wilkins, Baltimore, 1998.
28. Liebenson C, DeFranca C, Lefebvre R. Rehabilitation of the Spine: Functional Evaluation of the Cervical Spine, Williams & Wilkins, Baltimore, 1998.
29. Timm KE 1994. A randomized-control study of active and passive treatments for chronic low back pain following L5 laminectomy. JOSPT 20:276-286.
30. Manniche C, Lundberg E, et al. 1991: Intensive dynamic back exercises for chronic low back pain. Pain 47:53-63.
31. Morgan D. Concepts in functional training and postural stabilization for the low-back-injured. Top Acute Care Trauma Rehabil 1988;2(4):8-17.
32. Grabiner MD, Koh TJ, Ghazawi AE. Decoupling of bilateral paraspinal excitation in subjects with low back pain. Spine 17:1219, 1992.
33. Edgerton VR. Wolf SL, Levendowski DJ, Roy RR. Theoretical basis for patterning EMG amplitudes to assess muscle dysfunction. Med Sci Sp Exer 1996;28:744-751.
34. Paley C. A way forward for determining optimal aerobic exercise intensity? Physiotherapy 1997;83:620-624.
35. Janda V. Chapters 6 - Evaluaton of muscle imbalance in Liebenson C. Rehabilitation of the Spine: A Practitioner's Manual, Liebenson C (ed). Williams and Wilkins, Baltimore, 1996.
36. Vera-Garcia FJ, Gerneir SG, McGill SM. Abdominal muscle response during curl-ups on both stable and labile surfaces. Phys Ther 2000;80:564-569
Craig Liebenson,DC
Los Angeles, California
cldc@flash.net