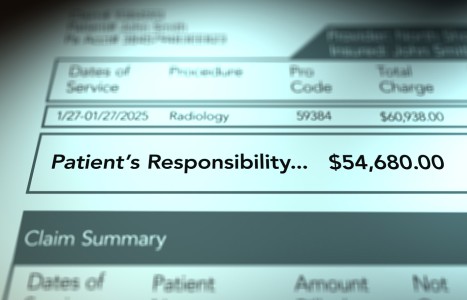
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Long-Term Consequences of Whiplash: Allergy; Breathing, Digestive and Cardiovascular Disorders; Hypertension and Low Back Pain
A recent paper out of Canada1 takes an intriguing look into what may be some of the less recognized features of the long-term consequences of whiplash trauma - a condition perhaps more rightfully referred to as cervical acceleration/deceleration (CAD) trauma. The authors, using data obtained by health surveys, attempted to correlate a history of neck injury from motor vehicle crashes (MVC) with chronic neck pain.
The authors reported that a history of neck injury was "positively associated with low intensity/low disability neck pain (OR= 2.81; 95% C1 1.81 -4.37), positively associated with high intensity/low disability neck pain (OR = 4.46; 95% CI 2.49-4.99) and with disabling neck pain (OR = 3.30; 95% CI 1.48-7.39)."
"Similarly," the authors continued: "We found a positive association between a history of neck injury in a motor vehicle collision and headaches that moderately/severely impact on one's health (OR = 2.09; 95% CI 1.27-3.44). No association was found between neck injury and depressive symptomatology (OR = 0.84; 95% CI 0.50-1.40). Our cross-sectional analysis suggests that neck pain and severe headaches are more prevalent in individuals with a history of neck injury from a car collision. However, the results should not be used to infer a causal relationship between whiplash and chronic neck pain and headaches."
This is a particularly interesting paper for me because the authors looked at something Drs. Michael Freeman, Anne Rossignol, and I looked at quite independently a few years earlier: a large case-control study we conducted involving over 700 people.2 We examined the attribution of MVC to chronic neck pain. We asked people with chronic neck pain if they would blame a prior MVC as the source of that pain. In that study, for which we have still not found a home (we were rejected by one epidemiological journal on the basis that the reviewers found our data incredible because, as they pointed out, whiplash injuries are "never chronic!"), we found an etiological fraction of 0.45. That means that 45 percent of patients with chronic neck pain attributed it to a prior MVC, most of which were whiplash injuries. As is the case with the present study, ours cannot be used to infer a causal relationship between whiplash and chronic neck pain based on the study design. However, it is likely that a substantial proportion of that attribution is valid; this would be consistent with the many outcome studies of whiplash injuries and the epidemiological work reported elsewhere.3,4
The authors begin this paper with references to the flawed Quebec Task Force on Whiplash-Associated Disorders paper, noting that it found that "the prognosis of neck injuries resulting from motor vehicle collision is favorable." As we pointed out in our 1998 paper in Spine,5 those conclusions could not possibly have been based on the literature they claimed to have relied upon. That criticism notwithstanding, this present paper is one of which we should all take notice.
After three mailings to their target population of 2,184 residents of Saskatchewan, the authors had 1,133 (55.1 percent) returned questionnaires. Normally, responses of less than 70 percent must be viewed cautiously because of the possibility of bias. For example, in a study such as this, some confounding factor might be operating such that it might cause people to be more or less likely to respond. If that were the case, the respondents might not be representative of all 2,184 residents in the original mailing. Countervailing this problem is the fairly large response. Moreover, there are ways to determine whether any such bias existed, and the authors assured us that their sample was probably representative, although the respondents were less likely to be younger, male, and unmarried.
The authors inquired about graded neck pain, headache, and depression. In the former two categories, the questions concerned symptoms in the past six months. In the case of depression, the questions concerned only the past week. One wonders why only the last week was considered in this protocol and whether, as in the case of the Beck Depression Inventory test, somatic complaints might have influenced the results.
Overall, 15.9 percent reported a history of neck injury from MVC. This was more common in females in all age groups. The authors also reported that those reporting neck injuries were more likely to be unmarried, have an annual income of less than $40,000 (I'm assuming this is in Canadian dollars), and be unemployed. One wonders again why these demographics were considered, since there is no compelling reason to relate unemployment or lower earning power with risk of injury in MVC, unless the unemployment was the result of such injuries. Might this be a subtle suggestion of secondary gain?
Perhaps the most important aspect of this study was the association of various comorbidities with history of neck injury from MVC. The authors looked at allergies, breathing disorders, hypertension, cardiovascular disorders, digestive disorders, and low back pain. They found higher comorbidities in all categories except hypertension; in many cases, the reported complaints were close to twice that seen in those with no history of neck injury. Moreover, the impact of these comorbidities was greater on the lives of those suffering neck injury than in those uninjured. They found that the general health of those having been injured was significantly lower than in those who had not. In the neck injury history group, 9.9 percent suffered from disabling neck pain in the six-month survey period vs. only 3.9 percent who had no history of neck injury. Headaches that moderately or severely affected the health were likewise more common among the MVC group (33 percent) than the non-MVC group (15.2 percent). As for depression, the numbers were similar: 32.8 vs. 19.3 percent, although later multivariate adjustment for confounders found the association attributable to other variables.
Unfortunately, the authors did not inquire about thyroid or other endocrine disorders. We had previously found a possible link between thyroid disease and CAD injury,6 and I know that one of the authors of the present study (Cassidy) knew about that paper because he wrote a critical letter to the editor of JMPT about it, despite the fact that we had acknowledged in the paper the shortcomings he criticized. In that study, we found a possible link between hypothyroidism and exposure to CAD trauma and speculated a hypothalamic injury as the cause. Again, no conclusive cause-and-effect connection can be drawn based on our study design, but papers such as this most recent one out of Canada offer more reason to investigate such connections further.
References
- Freeman MD, Croft AC, Rossignol AM. Chronic neck pain and whiplash: a case-control study of the relationship between acute whiplash injuries and chronic neck pain. Submitted for publication.
- Cote P, Cassidy JD, Carroll L. Is a lifetime history of neck injury in a traffic collision associated with prevalent neck pain, headache and depressive symptomatology? Accident Analysis and Prevention 2000:32:151-159.
- Croft AC. Whiplash: advanced topics. In Module 1 of Whiplash: the Masters' Program, Spring Valley, Spine Resea3. rch Institute of San Diego, 2000:96-99.
- Foreman SM, Croft AC (eds). Soft tissue injury: the long and short-term effects. Whiplash Injuries: the Cervical Acceleration/Deceleration Syndrome, second edition. Baltimore, Williams & Wilkins, 1995, 323-327.
- Freeman MD, Croft AC, Rossignol AM. "Whiplash Associated Disorders: redefining whiplash and its management" by the Quebec Task Force: a critical evaluation. Spine 1998:23(9):1043-1049
- Sehnert KW, Croft AC. Basal metabolic temperature vs. laboratory assessment in "posttraumatic hypothyroidism." JMPT 1996:19(1):6-12
Arthur Croft,DC,MS,FACO,FACFE
Director, Spine Research Institute of San Diego
San Diego, California
drcroft@san.rr.com