Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
The Assassination of a Hero
The following is from a forensic analysis review of a medicolegal case in which the plaintiff's attorney asked me to analyze the treating chiropractor's records. While the plaintiff won the low-impact case, the incomplete documentation led to what I refer to as "the assassination of a hero." I have always felt that doctors of chiropractic are heroes. They function, day-to-day, as true guardians of health; practicing with a drug-free, noninvasive, healthy lifestyle approach. I present this analysis for my colleagues as a form of critical review in the key elements of personal injury documentation.
Dear Mr. Attorney:
I would like to reply first with respect to your request that I review the aforementioned case, with particular regard to the most likely areas of attack by the defense counsel, and what I perceive would be your most sensible method of counterapproach.
The medical file on Jane Doe was submitted for my review on this date, and is limited to the following documents:
- Patient Intake Form(s) - Exhibit 1
- Auto/Work-Related Accident Form - Exhibit 2
- Pain Chart Form - Exhibit 3
- Clinical Final Exam Form - Exhibit 4
- Ranges of Motion Form - Exhibit 5
- Diagnosis/Prognosis Form - Exhibit 6
- Static EMG Testing - Exhibit 7
- Itemized Patient Ledger - Exhibit 8
- Narrative Final Report - Exhibit 9
Of immediate concern is the absence of certain documents required for file completeness: initial examination; treatment plan(s); outcome assessment forms; and daily chart notes. I did not find any interim examination(s); photographs (or drawings) of vehicle damage; a description of vehicles involved; or vehicle repair estimates to substantiate vehicular damage. I did not find any review of outside medical records (your client identifies having a family medical doctor, and provided the telephone number on the initial patient registration form). Such documentation is often needed in the medicolegal arena to substantiate the past medical history and the care (related to this injury) rendered.
Allow me to highlight areas of concern with respect to each of the above.
Patient Intake Form(s)
The patient registration form (intake form) doesn't indicate how the patient was referred to the chiropractor. The item was left blank. Did you, as the attorney of record, send her?
When was the lien obtained? I ask this because there is no insurance information completed, not even the patient's automobile insurance. In addition, the space for the response to "Name person ultimately responsible for account" was left blank. Was this patient aware that she was ultimately responsible for the bill? Or was she told that a lien would handle it? Did she ever receive a bill? Did she sign an exit disclosure statement of monies owed to the treating chiropractor for services rendered?
Auto/Work-Related Accident Form
The patient identifies that her vehicle has no airbags, but the final chiropractic narrative reported: "Airbags were not deployed." What type of vehicle hit the patient? The automobile insurance carrier was not identified, but the patient retained an attorney at the time of the initial office visit, which again points to the question: Was the client/patient aware of financial responsibility?
Pain Chart Form
The initial pain chart identifies right-sided neck and upper posterior shoulder ache as an eight (severe pain), and a mid-thoracic ache bilateral identified as a five (moderate pain). (I am attempting to explain the $600 fee on the initial visit; full spinal x-rays and full cervical x-rays, the initial exam fee, surface EMG and the therapy charges that are attached as subsequent charges.) I did not find any interim pain charts or outcome assessment forms that are generally obtained to monitor the patient's progress or response to each treatment plan.
Clinical Exam Forms - Final Exam
No patient identification or date has yet been identified as final examination. The records are incomplete in comparison to what a reasonably prudent doctor of similar scope of practice would perform and/or is required to perform: Data is lacking on visual evaluation; heart; lungs; postural studies; menstruation; muscle or myotome testing; shoulder and back orthopedic testing; and neurological testing is incomplete. The rule is simple. If it isn't documented, it never happened. Hence, it fails to substantiate the itemized billing.
Ranges of Motion - Final Exam
No patient identification, or date, identified as "final examination shoulder range of motion studies," was preformed. This is pertinent, because shoulder pain accompanied this patient's chief complaint on the initial patient registration form.
Diagnosis/Prognosis
After 14 months of care, the final diagnosis is subjective neck and back pain: cervicalgia and lumbago. It appears the patient ultimately diagnosed herself. Is this what she required treatment for? Is this the outcome of the 14 months of treatment rendered? This fails to substantiate the care rendered.
There is also a subluxation diagnosis for the cervical, thoracic and lumbar region. After 168 adjustments, do the clients/patients ever become subluxation-free? How does this differentiate a personal injury patient from every patient that enters a chiropractic practice? What happened to the initial pain complaints? Where is that diagnosis, and when did this patient develop low back pain? There is no documentation to withstand cross-examination of these issues.
I would try to explain in the clinical treatment record when this patient developed the lumbosacral pain that was reported upon in the final narrative, because the patient intake form only identifies neck and right shoulder pain. A change in condition, or a new condition, warrants an interim evaluation.
The doctor of chiropractic failed to itemize each and every complaint and assign each a diagnosis, and discuss any degree of resolution. (I may get into trouble with many of my colleagues on this point, but while everyone has subluxations and only a chiropractor may render this type of diagnosis, today's chiropractor is trained in differential diagnosis or a condition described by multiple diagnoses.) Differential diagnosis must be utilized in the PI arena.
Static EMG Testing
Who performed the surface EMG and provided its interpretation, and what is that individual's level of competency or certification with respect to this study? The final narrative assumes that person to be your treating chiropractor. The initial interpretation or diagnostic testing report is absent. Therefore, the charge is unsubstantiated without the diagnostic study. The same is true for the radiographs obtained; no diagnostic report is enclosed to record.
Itemized Patient Ledger
Point-in-fact: CPT code 97010 (hot/cold therapy) is generally recognized as a bundled code or part of another procedure, unless documentation to support the chiropractic necessity of its separate billing is provided. For example, when not just a heat pack, but heat treatment is used prior to manual therapy of stretching or trigger point release, that would justify its separate charge. CPT code 97010 was charged to this patient 48 times at $20 dollars per session, a charge of $960 (unsubstantiated by documentation).
The itemized client/patient ledger indicates separate charges for a range-of-motion exam, a neurological exam and an orthopedic exam. These charges are not identified as being separate from a service provided on the same day from those considered an integral part of the initial service performed. An example is 99203-05, the initial examination CPT coding utilized for visits (more on this later). The $600 charge for the initial office visit is unsubstantiated by documentation.
The itemized, reported final examination visit included passive care modalities charges, but the doctor reported that the patient "reached a point of maximum recovery" on this day, so the $80 for the therapy will not be perceived as "medically necessary," and is unsubstantiated by documentation. (The opening paragraph of final narrative report states that an initial and interim evaluation(s) have been preformed, yet itemized billing ledger fails to document such procedures.)
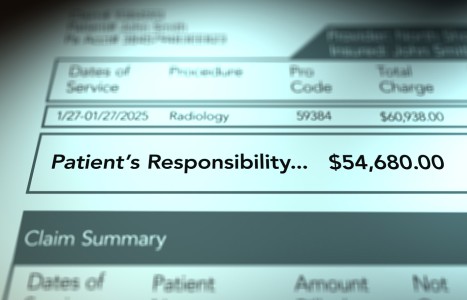
Fee Facts for the geographical area reports fees are well above the 90th percentile. A total of $2,655 is not justified, based upon the documentation submitted for my review, and is subject to review by opposing counsel.
Narrative Final Evaluation
The opening paragraph states that an initial and interim evaluation(s) were preformed. Please forward these records. I would also request the daily chart notes to assist me in the documentation of substantiating the injuries sustained, and the itemized billing before defense counsel attacks these. It is from these documents and the outcome assessment forms that the final diagnosis and concluding prognosis is also determined. This is how the professional opinion of the treating chiropractor is established.
Interim exams should be performed every four to six weeks until the patient is significantly improved, quarterly thereafter and upon discharge, having reached maximum chiropractic improvement (MCI). Each interim (objective) examination needs to have supporting evidence of your client/patient's subjective complaints at these intervals; neck disability index; pain drawings; and activities of daily living forms. Preferably, these should be completed and signed by your client.
The final narrative report fails to contain certain elements. Those lacking are identified as: a one-paragraph history for a biomechanical picture; relative weight of vehicles; forces of impact; initial complaints at scene and during the first examination; and the past medical history for pre-existing conditions. (If medical records were not obtained, how can the chiropractor state that no pre-existing condition was present? Merely quoting the patient won't do it in a court of law!) The physical examination findings (initial, interim, and final evaluation); the review of records; each and every complaint is to be itemized and assigned a diagnosis. The loss of earnings; the occupation description; the personal injury's effect on job performance and its effect on the client's activities of daily living, and any specific lifestyle changes, must also be reported.
The final examination report fails to discuss the treatment program administered and any changes to the original treatment plan, once the patient failed to respond clinically. Supporting evidence is required because the client/patient's itemized ledger identifies a continuance of passive care and physical therapy modalities for well over a year.
The final evaluation fails to discuss the prognosis of every original presenting complaint. For example, the patient's primary complaints were related to her neck and right shoulder. The patient reported on the initial intake form that the symptoms were getting worse and interfering with work and sleep, and it hurt to turn her neck. What had been the progression of improvement?
The treating chiropractor failed to substantiate the need for provisions of any future medical care. The treating chiropractor's reported future medical estimate of an untoward $5,700 is unsubstantiated. In requesting future medical provisions, did the treating chiropractor fail to discuss other medical options available to your client/patient (e.g., magnetic resonance imaging, orthopedic referral or pain management centers)? If the treating chiropractor doesn't do it or request its provisions, you can bet the defense counsel will bring it up. (There's nothing like planting the seeds of doubt about our "hero's" capability and professional opinion!)
In the "factors of permanent disability" section, the treating chiropractor states that his opinion is based on the final examination, the previous records, and the patient's subjective complaints. It is difficult to state a case on range of motion studies and subjective complaints alone to substantiate factors of permanent disability. The Mercy Guidelines state: " Functional outcome assessments of everyday tasks are very suitable for evaluating treatment of dysfunctions of the neuromusculo-skeletal system." (My emphasis.) "Many questionnaires could be used. (Recommendation 10.1, Pg. 151, Rating: Established.)"
Easy-to-understand manifestations of injury and impairment will bolster a claim and possibly assist in generating a settlement. If no settlement is achieved, the treating chiropractor will be asked at trial to describe to a jury what impact the patient's condition had on her life. Without adequate documentation, few witnesses (chiropractors) have sufficient recall to testify either accurately or effectively.
The submitted final narrative report fails to substantiate the $300 fee for CPT code 99080. These codes have components that need to be satisfied. Who requested the narrative report? Commonly, the report is not reimbursable unless a medicolegal report is requested; only the final examination charge is reimbursable. The report then becomes a component of the final E/M code, to substantiate the "medical /chiropractic necessity" of the final examination.
The typical profile for a motor vehicle accident case that is forced to trial by the insurance company includes, but is not limited to, features such as:
- minor property damage to the vehicle;
- the patient having had prior problems, with symptoms solely due to pre-existing problems;
- not enough force to cause any injury;
- excessive treatment; or
- the medical/chiropractic treatment is inconsistent with the injuries originally alleged by the plaintiff.
One might inquire whether the expense of the repeated adjustments three times per week over long periods of time, at $60-90 a visit, plus expensive x-rays and traction after one year would, in the eyes of opposing counsel, be considered excessive treatment.
Skepticism is a means to opening the door. If the jury has skepticism, the insurance company has skepticism; the defense attorney has skepticism; and then wants a trial. Any chiropractor will admit that some members of the professional and general public are a tad skeptical about various aspects of chiropractic, regardless of how unwarranted that skepticism might arguably be. I would advise the treating chiropractor to be prepared for this skepticism, prior to court appearance, by an informal self-review of the chart notes and treatment plan placed into a calendar format.
Colleagues: As doctors of chiropractic - like it or not - an implicit part of your duty to the patient is accurate and adequate record-keeping. Perhaps the most important reason for documentation is to provide timely and effective care for your patient. Beyond that, you must accept the fact that other parties may be paying for your services and have a right to know what they are reimbursing you for, as well as to the probable diagnosis and prognosis.
On litigated cases, all parties require a final narrative report, which becomes crucial to the settlement of the case. The chiropractor is required to outline levels of disability, the likely need for future care, surgery, etc. This final narrative is the single most important tool the plaintiff attorney has with which to construct the demand letter. If it is understandable; organized; concise; readable; and believable, it is much more likely that the case will settle. That means that one day the chiropractor will be paid on the personal injury lien, and not have to brother with arbitrations or court appearances. Furthermore, final narratives should only be sent out at the end of the case, when requested by the attorney in writing. You can't expect to be paid for something if it wasn't requested.
I won't belabor this point further. It is sufficient to say that the chiropractor should keep patient charts as organized as possible. However you organize your charts, just remember that medicolegal charts are just short of public domain, in that your charts will often be subpoenaed for photocopying purposes. A good rule in the medicolegal arena that the treating doctor should follow is to always request the previous treating doctor's records, in particular, the diagnostic records.
The first step in patient care is to provide a diagnosis. The same patient could have the same condition described in multiple ways. The standard system of coding diagnoses is called the International Classification of Diseases, Clinical Modification (ICD-CM). Several university websites offer access to ICD-9-CM codes on line (http://www.mcis.duke.edu/standards/termcode/icd9/). Pay particular attention to the tabular section on musculoskeletal codes. Most of the ICD-CM manuals are arranged in two parts, the first part listing conditions alphabetically (tabular), and the second listing them by number. Find a condition that is reasonably close to the one being treated, look up the number provided, and you will be somewhere in the area of the exact condition you're looking for. When the insurance company or attorney receives the itemized statement or HCFA claim form, accompanied by its report, using the most accurate code indicates to them the nature of the visit in a more specific manner and tells them what you found.
The second step is in telling what you did. CPT (current procedural terminology) codes are published and copyrighted by the American Medical Association. (Bet you didn't know that!) and identify the set of services provided to the patient.
There are codes to describe the initial visit, report-of-findings visit, and interim exam visits (called E/M visits, or evaluation management visits). Chart documentation is the key in this arena. Generally, if the patient has a new complaint or condition that worsens, it needs evaluation and management.
The trick is to determine which of the five levels (I-V) of E/M visits to use. Suffice it to say that a host of factors are used in determining this, such as time spent with the patient, the difficulty of the condition or complaint. I won't go into detail here. A word of caution however, is indicated. Ever wonder why certain insurance companies (you know whom I mean), "down-code" chiropractors' E/M codes and routinely reimburse lower? Consider what you need in your chart note to assure that you can continue to provide high-quality chiropractic care to your patients and still satisfy billing requirements. Always practice good record-keeping!
Nancy Molina, DC
San Juan Capistrano, California