It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Metabolic Syndrome: An Ongoing Health Care Disaster
- Type 2 diabetes is clearly a potential outcome of MetS, but the list of related conditions is stunningly broad and seldom discussed.
- A blood panel that includes CMP-14, CBC, lipids, HbA1c, basic thyroid, CRP, ferritin, fibrinogen, uric acid, homocysteine, vitamin D, phosphorus, and fasting insulin is a good diagnostic starting point for most patients.
- Helpful supplements include B vitamins, ashwagandha, magnesium, zinc, chromium, berberine, lipoic acid, omega-3 fatty acids, curcumin, boswellia, nattokinase, taurine, ECGC, L-carnitine and numerous others based on individuality.
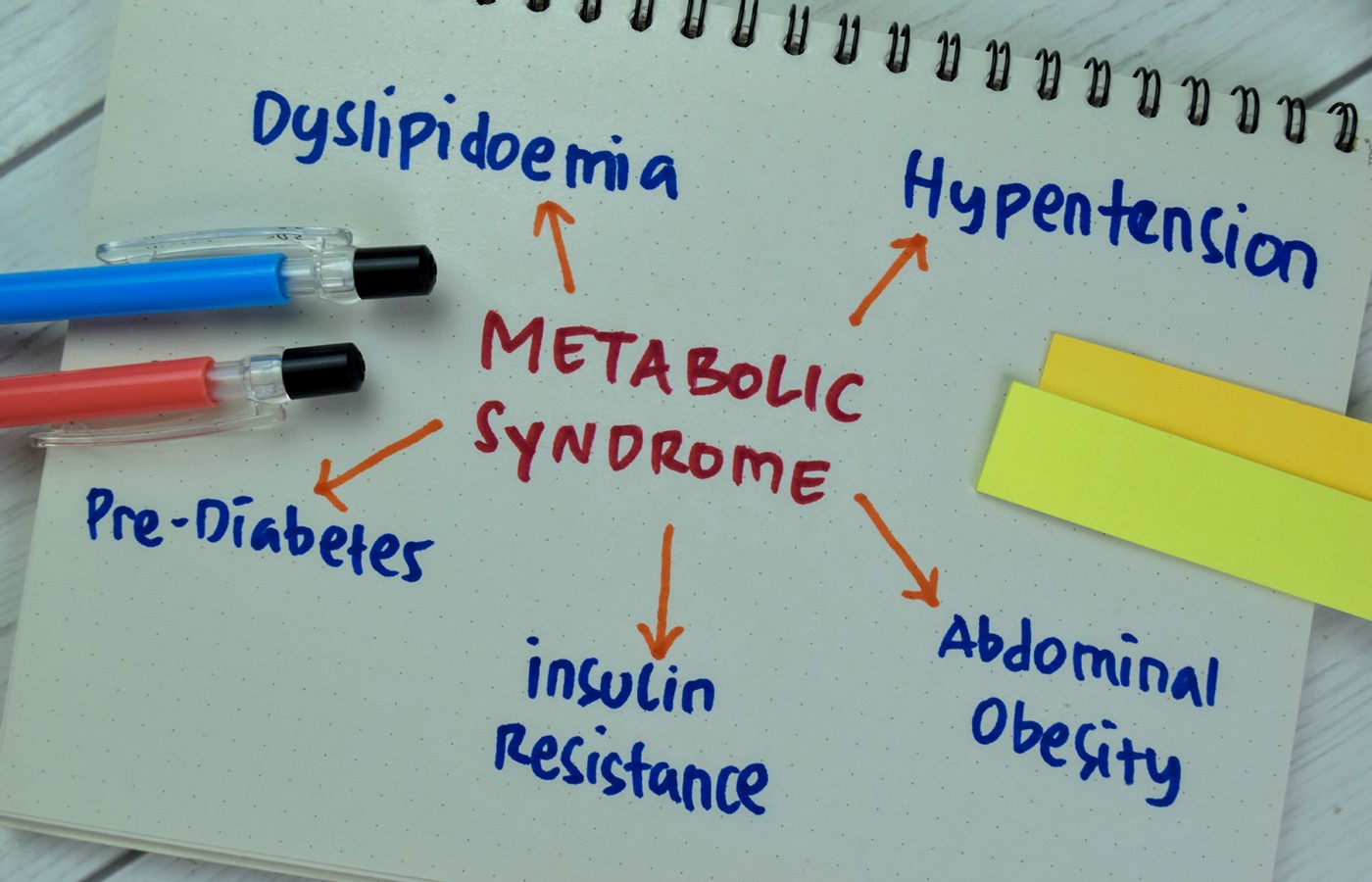
Metabolic syndrome is a complex disorder based on aberrant glucose metabolism involving numerous coexisting and interconnected conditions. With approximately 100 million Americans (35% of adults)1 suffering from the multitude of its far-reaching effects, it couldn’t be more relevant to our current collective health and well-being.
Metabolic syndrome (MetS), sometimes simplistically equated with pre-diabetes, is a far more complex and deeply destructive disorder. Identified in 1988 by Dr. Gerald Reaven, Syndrome X2, as he first called it, involves insulin resistance – an increased production of insulin is needed to accomplish the job of maintaining normal glucose metabolism. Insulin, however, is not an innocuous substance because excess amounts of this hormone create an environment that is seriously unhealthy.3-4
A Very Simplified View of Cause and Effect
Cause – Diet is key. Excessive refined carbohydrates, added sugars and other highly processed foods (HPFs) are the main culprits.5
Effect - Excess triglycerides, one of the hallmarks of metabolic syndrome, are generated by excessive carbohydrate intake and block the hormone leptin, which influences appetite and satiety, from passing through the blood brain barrier.6 More hunger ensues. It has been demonstrated that HPFs can be highly addictive.7
Many patients respond well when given an understandable account of what they are facing and have an added capacity to understand what lies ahead if they continue on the same path. At the very least, they are informed.
Diagnostic Criteria
Metabolic syndrome is diagnosed when a person has three or more of these conditions:
- Central or abdominal obesity, reflecting visceral fat (measured by waist circumference). Men: greater than 40 inches; women: greater than 35 inches.
- High triglycerides – 150 milligrams per deciliter (mg/dL) or more, or you’re taking medicine for high triglycerides.
- Low HDL cholesterol. Men: less than 40 mg/dL; women: less than 50 mg/dL, or you’re taking medicine for low HDL cholesterol.
- High blood pressure – 130/85 (mmHg) or more, or you’re taking medicine for high blood pressure.
- High fasting glucose – 100 mg/dL or more, or you’re taking medicine for high blood glucose.8
Interrelated Conditions
Type 2 diabetes is clearly a potential outcome of MetS, but the list of related conditions is stunningly broad and seldom discussed. Individuals vary, but they may also be affected by a greatly increased risk for cardiovascular disease including atherosclerosis, hypertension and lipid abnormalities,9 fatty liver,10 systematic inflammation,11 sex hormone derangements,12 a pro-cancer environment,11 hypothyroid,13 calcium / phosphorus imbalance,14 increased coagulation,15 immune system dysfunction including increased risk of viral infection,16 dysregulation of the microbiome,17 autonomic nervous system dysfunction,4 particularly excess cortisol and adrenaline, and other neurotransmitter issues.18
A list of what isn’t affected might be shorter. MetS is not the only potential cause of any of these conditions; however, all have been linked to it.
Obesity Statistics in Adults & Children
According to CDC statistics, in the past 60 years obesity and severe obesity rates for adults have sharply increased from 13.4 to 42.8% and 0.9 to 9.1%, respectively. Children and teens had 4% to 20.7% and 6.1% to 22.2% increases in obesity, respectively, for the same time frame.19-20
Insulin Impact
The Quebec Study found that an insulin level of 13 uIU/mL correlated with an eightfold higher heart attack risk than a level of 9.3 uIU/mL (reference range: 0-24.9 uIU/mL).3
Insulin levels in Kitava average 3-6 uIU/mL, which does not increase with age. Healthy carbohydrates are a staple, while intake of highly processed Western food is negligible. Stroke and ischemic heart disease are absent or rare.21
Insulin resistance can cause global autonomic dysfunction, involving sympathetic overactivity, which increases along with worsening glucose metabolic impairment.4
Highly Processed Foods and Addiction
Highly processed foods (HPFs) have been demonstrated to be addictive substances. Substantial public health costs are associated with a food supply dominated by cheap and heavily marketed HPFs.22 Additionally, recent research has shown an association between artificial sweeteners, also considered HPFs, and a substantially increased risk of depression.23
Basic Blood Testing
A panel that includes CMP-14, CBC, lipids, HbA1c, basic thyroid, CRP, ferritin, fibrinogen, uric acid, homocysteine, vitamin D, phosphorus, and fasting insulin is a good starting point for most patients. Testing can be expanded as needed with the consideration that resolving fundamental issues often improves concomitant conditions as well.
Potential Solutions / Discussion
The concept of metabolic syndrome dates back at least to 1864 when a layperson in London, William Banting, wrote his Letter on Corpulence outlining a similar scenario. He established that a high-sugar, high-carb diet was the cause of his obesity. In 1972, Dr. Atkins’ Diet Revolution identified the same target, excess carbohydrates.
Contemporary diet programs also address the carbohydrate issue and can be a part of an individualized treatment plan. Exercise is surely beneficial,24 but diet is essential. Restricting carbohydrates can be uncomfortable for a few days, but the cravings will subside.
Helpful supplements include B vitamins, ashwagandha, magnesium, zinc, chromium, berberine, lipoic acid, omega-3 fatty acids, curcumin, boswellia, nattokinase, taurine, ECGC, L-carnitine and numerous others based on individuality. Leading supplement companies have formulated products that are excellent.
A good possibility for a long-term solution is The Healthy Eating Pyramid, from The Nutrition Source, Department of Nutrition, Harvard T.H. Chan School of Public Health.25
Historically, diet pills such as amphetamines, Phen-Fen and ephedra have failed, sometimes disastrously. Time will tell if the latest, semaglutides, will break that mold. A new supplement, an extract of hops, may offer an option to curb hunger moving forward.
If metabolic syndrome is not successfully resolved with a holistic treatment plan that addresses the root cause and significant concomitant conditions, the patient may require an increasing number of prescription medications to deal with myriad worsening symptoms.
We know what the issues are and what is at stake, yet there is no urgency to bring this to the forefront and have a national discussion. The serious issues in our food supply, the failure to add warning labels concerning the harmful and addictive nature of certain foods, and the backburner mentality will continue escalating metabolic syndrome’s disastrous effects on the American population. We can and must do better.
References
- Aguilar M, Bhuket T, Torres S, et al. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA, 2015 May 19;313(19):1973-4.
- Reaven GM. Syndrome x: a short history. Ochsner J, 2001 Jul;3(3):124-5.
- Després JP, Lamarche B, Mauriège P, et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med, 1996 Apr 11;334(15):952-7.
- Perciaccante A, Fiorentini A, Paris A, et al. Circadian rhythm of the autonomic nervous system in insulin resistant subjects with normoglycemia, impaired fasting glycemia, impaired glucose tolerance, type 2 diabetes mellitus. BMC Cardiovasc Disord, 2006,6:19.
- Canhada SL, Vigo Á, Luft VC, et al. Ultra-processed food consumption and increased risk of metabolic syndrome in adults: The ELSA-Brasil. Diabetes Care, 2023 Feb 1;46(2):369-376.
- Banks WA, Coon AB, Robinson SM, et al. Triglycerides induce leptin resistance at the blood-brain barrier. Diabetes, 2004 May;53(5):1253-60.
- GearhardtAN,DiFeliceantonioAG.Highly processed foods can be considered addictive substances based on established scientific criteria.Addiction,2023;118(4):589-598.
- Grundy SM, et al. Diagnosis and management of the metabolic syndrome. Circulation, 2005 Oct;112(17):25.
- Alshehri AM. Metabolic syndrome and cardiovascular risk. J Family Community Med, 2010 May;17(2):73-8.
- Goyal A, et al. Prevalence of fatty liver in metabolic syndrome. J Family Med Primary Care, 2020 July; 9(7):3246-3250.
- Gugliucci A. Chapter one - biomarkers of dysfunctional visceral fat. Advances Clin Chem, 2022;109:1-30.
- Pitteloud N, et al. Increasing insulin resistance is associated with a decrease in Leydig cell testosterone secretion in men. J Clin Endocrinol Metab, 2005 May;90(5)2636-2641.
- Khatiwada S, Sah SK, Kc R, et al. Thyroid dysfunction in metabolic syndrome patients and its relationship with components of metabolic syndrome. Clin Diabetes Endocrinol, 2016 Feb 1;2:3.
- Page ME. Degeneration, Regeneration. Biochemical Research Foundation, 1949.
- Nieuwdorp M, Stroes ES, Meijers JC, Büller H. Hypercoagulability in the metabolic syndrome. Curr Opin Pharmacol, 2005 Apr;5(2):155-9.
- Geerling E, Hameed M, Weger-Lucarelli J, Pinto AK. Metabolic syndrome and aberrant immune responses to viral infection and vaccination: Insights from small animal models. Front Immunol, 2022;13:1015563.
- Wang PX, Deng XR, Zhang CH, Yuan HJ. Gut microbiota and metabolic syndrome. Chin Med J, 2020 Apr 5;133(7):808-816.
- Muldoon MF, Mackey RH, Korytkowski MT, et al. The metabolic syndrome is associated with reduced central serotonergic responsivity in healthy community volunteers. J Clin Endocrinol Metab, 2006 Feb;91(2):718-21.
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960-1962 through 2017-2018. NCHS Health E-Stats, 2020.
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963-1965 through 2017-2018. NCHS Health E-Stats, 2020
- Lindeberg S, Eliasson M, Lindahl B, Ahrén B. Low serum insulin in traditional Pacific Islanders - the Kitava Study. Metabolism, 1999 Oct;48(10):1216-9.
- GearhardtAN,DiFeliceantonioAG.Highly processed foods can be considered addictive substances based on established scientific criteria.Addiction, 2023;118(4):589-598.
- Samuthpongtorn C,Nguyen LH,Okereke OI, et al. Consumption of ultraprocessed food and risk of depression.JAMA Netw Open,2023;6(9):e2334770.
- Golbidi S, Mesdaghinia A, Laher I. Exercise in the metabolic syndrome. Oxid Med Cell Longev, 2012;2012:349710.
- The Nutrition Source, Department of Nutrition, Harvard T.H. Chan School of Public Health; andWillett WC, Skerrett PJ. Eat, Drink, and Be Healthy. Free Press/Simon & Schuster Inc., 2005.