New York's highest court of appeals has held that no-fault insurers cannot deny no-fault benefits where they unilaterally determine that a provider has committed misconduct based upon alleged fraudulent conduct. The Court held that this authority belongs solely to state regulators, specifically New York's Board of Regents, which oversees professional licensing and discipline. This follows a similar recent ruling in Florida reported in this publication.
Managing Osteoporosis: What DCs Can Offer
Editor's Note: This is part 2 of a two-part article. Part 1 ("Diagnosing Osteoporosis: It's Not Just About DXA" appeared in the November issue.
Chiropractors have much to offer in managing the treatment of osteoporosis. Of course, we can't manage the pharmaceutical intervention, but we can certainly manage the nutritional, exercise and fall-prevention pieces of this very complex, but frightfully common disorder.
Chiropractors are uniquely trained to manage both nutrition and exercise. We all have patients with osteoporosis or osteopenia. A 2019 position paper published in Osteoporosis International reveals that diagnosis and treatment of osteoporosis have many issues and pitfalls; patients can easily fall through the cracks.
The lifetime incidence of osteoporotic hip fractures is remarkably high and lies within the range of 40-50 percent in women and 13-22 percent for men. The mortality at one year post-fracture has traditionally been reported as 30 percent13 and more recently described as "around a third within a year."14
Patient Management: The Three Staples
We can help patients avoid this potentially tragic event by managing the nutritional and exercise / fall prevention aspects of their treatment. I will not cover nutrition in this article, as it is a very broad subject and there are those who have more expertise in this subject. Exercise or physical rehabilitation and fall prevention is again a topic that many have more expertise than I do. However, very little research has been conducted to examine the effectiveness of physical rehabilitation measures designed specifically to prevent osteoporotic fractures. Most of the research has been focused on drug intervention intended to reverse or prevent the loss of bone mass.
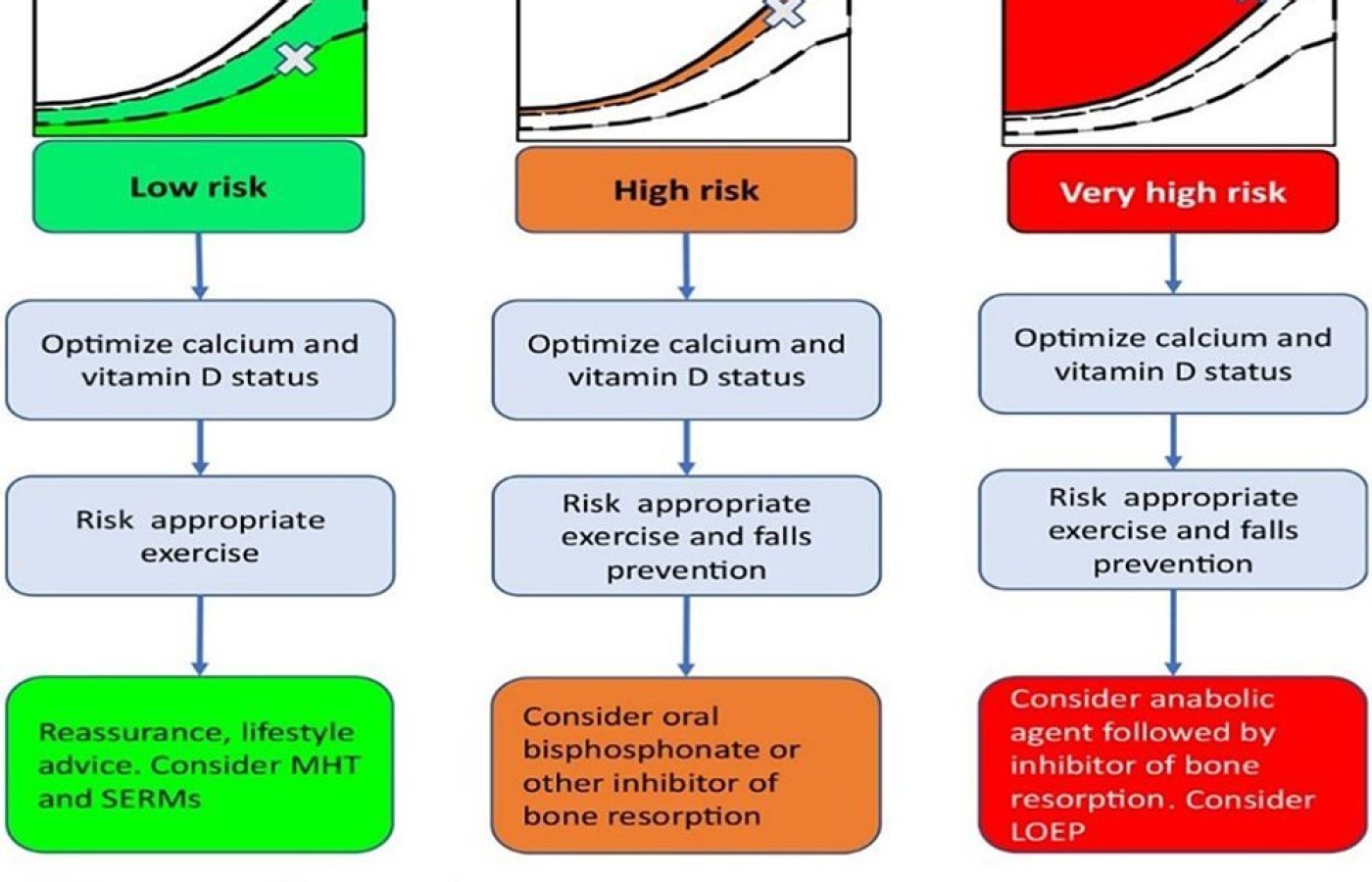
This algorithm is from a position paper published in November 2019 in Osteoporosis International. It is open access. Notice that all the treatment pathways include: optimize calcium and vitamin D status, and risk-appropriate exercise. Then there is the addition of fall prevention in the higher-risk categories. I don't know why they didn't include that in the low-risk category as well. But I also would not use the phrase optimize calcium and vitamin D status; I would call it nutritional counseling and support.
Focusing on Exercise
The role of exercise relative to building bone mass or preventing bone loss has only recently received attention. The majority of the strategies have been designed to elicit a sufficient weight-bearing load to stimulate bone growth without creating excessive strain or risk for fracture.
Unfortunately, to date there is no consensus on what constitutes the best rehab / exercise "formula" for osteoporosis.15 But there is now more interest in researching which exercise practices are more beneficial than others.16
Every patient with osteoporosis needs to do some form of weight-bearing exercise.17 However, it is rare that exercising alone will replace bone. In fact, most studies on exercise show only a few percentage differences in BMD. An increase in BMD does not necessarily translate to bone strength. There actually may even be a difference between load-induced bone formation and pharmaceutically induced bone formation.
Because of the complexity of bone and risk factors associated with fractures, the best approach should be to adopt a wide preventive regime, rather than a narrow focus on increasing bone mass. Balance and conditioning will reduce the risk of fractures.
Chiropractors have the unique expertise of being able to council patients on both nutrition and rehabilitative exercise programs. As with most patients, one size does not fit all. The patient needs to buy into the exercise regime and incorporate it into their lifestyle along with a healthy diet. We have specialists in the fields of nutrition (DACBN, DACBCN) and physical rehabilitation (DACBSP, CCSP) that one can consult, if you personally are not prepared to manage all the aspects in the care of osteoporotic patients.
Clinical Recommendations
Exercise Programs That Might Be Helpful |
| Below is a list of exercises with some recent data that indicate they can help reduce or reverse bone loss: |
This is not by any means an exhaustive list, but it should give you a good starting point if you need one. |
Please do not recommend that the patient just do a random weight-bearing exercise or give them a video and send them on their way. Patients need to be monitored and coached on how to perform rehabilitative exercise, and counseled on nutrition. Depending on your own experience and expertise, you most likely have a bias toward certain exercise programs. I am not an expert on exercise physiology; but I can share with you what I have recommended to patients and colleagues for the management of osteoporosis.
Lani Simpson, DC, CCD (https://lanisimpson.com/) has written a great book on osteoporosis and has a plethora of information on her website, including a short video discussing the different forms of exercise for osteoporosis. I have referred patients and colleagues alike to consult her expertise. Below are a few recommendations for clinicians to consider in the management and treatment of patients with osteoporosis:
1. Check the DXA scan to determine if it has been done well. They are not difficult to read and one can review how to read them on this site: https://rdcu.be/b6qPO. This will not make you an expert, but it will give you an understanding of how these scans are performed and read.
Errors in positioning, anatomical variants, artifacts, and averaging the density of L1-L4 are possible. Errors can even occur with the information used for the data comparison such as gender, age and ethnicity. How many times have you found an error in spelling or checking the wrong box? If something doesn't look right, it should be reviewed.
Also, review the FRAX score or do it again just to confirm. If the patient has a TBS score, add that to the FRAX score. If something doesn't seem right, get a second opinion. You might save a patient or two from being put on medication for years.
2. Diet and nutrition counseling. This needs to be tailored to the patient, depending on what other medical issues that patient may have.
3. Initiate an exercise program which focuses on posture, balance and conditioning first. Posture and balance are key to preventing falls, along with good conditioning. The patient needs to have an active role in choosing their options. Performing exercise in a mindful way is important for balance. I personally like to use a combination of mindful exercise; for instance, tai chi, Iyengar yoga, Feldenkrais, even Pilates. You probably have a favorite. Add mindful exercise to weight-training, cross training or aerobic weight-bearing exercise.
If you don't have the time or the expertise; refer the patient to one of your colleagues who does. We have chiropractic specialties in the fields of nutrition and sports medicine, of course many others. Refer to our colleagues in our own profession.
References
13. Moran CG, et al. Early mortality after hip fracture: is delay before surgery important?. J Bone Joint Surg Am, 2005;87(3):483-489.
14. National Hip Fracture Database Annual Report 2017.
15. Shojaa M, et al. Effect of exercise training on bone mineral density in post-menopausal women: a systematic review and meta-analysis of intervention studies. Front Physiol, 2020;11:652.
16. Zhang Y, et al. Effects of mind-body exercises for osteoporosis in older adults: protocol for systematic review and Bayesian network meta-analysis of randomized controlled trials. Medicine, 2020 Mar;99(11):e19426.
17. Daly RM, et al. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther, 2019;23(2):170-180.