It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
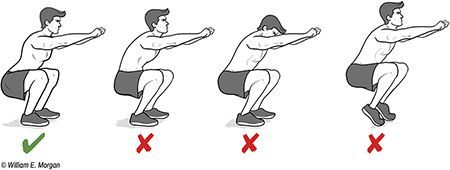
Essentials of Assessment: The Squat
The squat is a simple, fast and functional tool to evaluate patient symmetry and function. As simple and easy as it is to implement, it can yield considerable amounts of valuable, clinically relevant information.
A properly executed squat uses an aggregate of several joints (including ankles, knees, hips and spine) and muscles (too numerous to mention here). While a normal squat will validate a normal functional movement pattern, an abnormal squat may lead to additional evaluations to tease out the dysfunction. Muscle weakness or tightness, instability and reduced joint motion can all be teased out with this valuable diagnostic tool.
Why should you include the squat in your patient assessment? One reason is that the squat is a normal motion pattern – part of the activities of daily living. Indeed, one of the factors which results in infirmity and the need to move into assisted living is the inability to squat. We squat hundreds of times per day: getting in and out of a car, sitting in a chair, accessing items from the floor or shelves, exercising, and using the commode.

There are several methods for evaluating the squat, each with sound arguments for use. Every advocate for evaluating squatting motions has a favorite variation: back squat, front squat, single-leg squat, overhead squat, single-leg box squat, or some other variant. For simplicity, we will start with the fundamental air squat.
Prior to performing a squat, we should ensure the patient can safely perform a squat by ruling out any orthopedic injury, age-related exclusion or other contraindication for squatting. While a squat may be an important tool for evaluating a teenage soccer player, it isn't for a geriatric patient using a walker.
Patient Instructions for Performing This Evaluation
- Stand with your heels shoulder-width apart and toes pointed forward or slightly out (not more than 10 degrees of external rotation).
- Squat down until your thighs are at least parallel with the ground.
- Perform three repetitions while I observe from the front, then three repetitions while I observe from the side, and then three more while I stand behind you.
I should note that I allow the patient to extend their arms forward as a counter lever, but do not require it.
A Normal Squat Will Have These Characteristics
- Symmetry: the patient will not swerve to one side.
- The heels and the toes will remain on the ground; the feet will not rotate.
- The knees will not travel forward of the toes.
- Lumbar lordosis will be maintained throughout the squat.
- The head will remain up and neutral to slightly extended, but not flexed or hyperextended.
- Normal ankle dorsiflexion will be observed.
- Hip and knee motion should be fluid, pain-free, and demonstrate movement throughout the ranges required to perform a squat.
- The knees should descend in alignment with the tibias and not travel medially into a valgus position.
What Can the Squat Tell Us?
Head alignment and gaze: If the patient is not able to comfortably hold his/her head up during the squat, it may be indicative of a spinal injury or loss of flexibility of the thoracic or cervical spine. If the neck hyperextends during the squat, it may be a compensation for loss of thoracic motion. Treatment of faulty head position can include spinal adjustments, supported by strengthening or mobility exercise, and coaching the patient in squatting techniques.
Thoracic spine and chest (thorax): The thorax is best evaluated from a lateral position. The thorax should remain stiff and neutral throughout the squatting motion. The chest should be held upward. Curling forward of the thoracic spine and lowering of the chest during the squat may indicate a motor control malady. This can occur from postural protraction of the shoulders, hyperkyphosis of the thoracic spine, muscular weakness of the paraspinal muscles or scapular retractors, or tightness of the scapular protractors.
Lumbar spine: The lumbar spine should be held in a neutral lordosis throughout the squat. Inability to hold the lumbar lordosis throughout the squat can result from weakness of the paraspinal muscles, acetabular restriction (capsular tightness, a deep hip socket, degenerative joint disease of the hip or cam deformation), lack of lumbar spine mobility or muscular imbalances (weak or tight muscles).
Hip position: Excessive abduction of the hips may indicate a bony defect in the hip joint, muscular imbalance of the gluteal complex (weakness, tightness or motor control disparity) or reduced dorsiflexion of the feet.
An asymmetrical shifting to one side as viewed in the frontal plane may indicate asymmetry of strength, flexibility and hip motion.
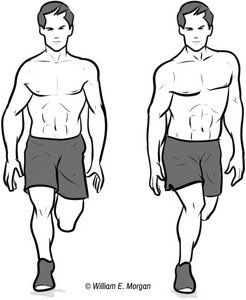
Knee motion: Valgus position of the knees during squatting is indicative of weakness or inhibition of the gluteus maximus and other external rotators of the hip. If I suspect gluteus maximus weakness and the patient is able to tolerate this test, I ask them to perform a single-leg squat (Figure 2).
If the knee passes far in front of the toes when viewed from the side, it can indicate gluteus maximus or hamstring weakness, or quadriceps-dominant squatting motions. It also may be a sign of reduced knee motion in the sagittal plane.
Foot motion: If the feet externally rotate during the squat, this is strongly associated with a loss of normal dorsiflexion. It may be due to tightness of the gastrocnemius and/or soleus, or loss of accessory motion of the joints of the foot. Stretching and/or foot adjustments may be indicated.
Advanced Squat Assessments
In addition to observing unloaded two legged squats, there are variants that can be used to assess our more athletic patients. The single-leg squat is a simple and efficient way to assess gluteus maximus function in the clinic, especially for more athletic patients.
Observe the patient in the frontal plane while he/she squats with one leg held up and posterior. If the ipsilateral knee migrates to a valgus position or if the contralateral pelvis drops, you may suspect weakness of the gluteus maximus on the side of weight-bearing. This is predictive for a predisposition of anterior cruciate ligament (ACL) injury.
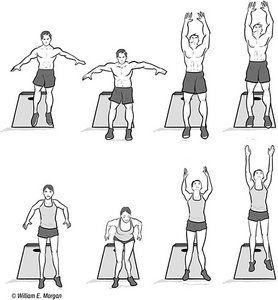
Another more dynamic test reserved for athletes involves the vertical drop jump. The vertical drop jump is performed by having the athlete jump off a platform 31 cm high with the feet 35 cm apart into a squat, then jump back into the air (Figure 3). If the knees manifest a valgus position as the athlete lands, it indicates a predisposition for ACL injury. Female athletes are particularly susceptible to this finding and are also much more likely to suffer from ACL disruption.
The Take-Home
Squat assessments are valuable clinical tools for helping identify biomechanical deficits and can help determine which sites would benefit from adjustments, exercise, neuromuscular training or mobility training. Squats are particularly beneficial for analyzing patients who wish to participate in rigorous activities. The squat is a functional movement complex used in many activities of daily living and also in athletics.
The NSCA has a great resource on assessing the back squat ("The Back Squat: A Proposed Assessment of Functional Deficits and Technical Factors That Limit Performance"), which I highly recommend if you'd like to learn more on this topic.
Resources / Suggested Reading
- Myer GD, Kushner AM, et al. The back squat: a proposed assessment of functional deficits and technical factors that limit performance. Strength & Conditioning J, 2014;36:4-27.
- Myer GD, Brent JL, Ford KR, Hewett TE. Real-time assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. Strength & Conditioning J, 2011;33:21-35.
- Kushner AM, Brent JL, Schoenfeld B, Hugentobler J, Lloyd RS, Vermeil A, Chu DA, McGill SM, and Myer GD. The back squat: Targeted training techniques to correct functional performance deficits and teach proficiency. Strength and Conditioning Journal. 2015.
- Myer GD, Ford KR, Khoury J, Succop P, and Hewett TE. Biomechanics laboratory based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med, 2011;45:245-252.
- Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower extremity biomechanics in female athletes. J Strength Cond Res, 2005;19:51-60.
- McKean MR, Dunn PK, and Burkett BJ. The lumbar and sacrum movement pattern during the back squat exercise. J Strength Cond Res, 2010;24:2731-2741.
- McGill SM, Norman RW. Dynamically and statically determined low back moments during lifting. J Biomech, 1985;18:877-885.
- List R, Gulay T, Stoop M, and Lorenzetti S. Kinematics of the trunk and the lower extremities during restricted and unrestricted squats. J Strength Cond Res, 2013;27:1529-1538.
- McLean SG, Felin RE, Suedekum N, et al. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc, 2007;39:502-514.
- Rahnama N, Reilly T, Lees A. Injury risk associated with playing actions during competitive soccer. Br J Sports Med, 2002;36:354-359.
- Rodacki AL, Fowler NE, Bennett SJ. Vertical jump coordination: fatigue effects. Med Sci Sports Exerc, 2002;34:105-116.
- Orishimo KF, Kremenic IJ. Effect of fatigue on single-leg hop landing biomechanics. J Appl Biomech, 2006;22:245-254.
- Prodromos CC, Han Y, Rogowski J, et al. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy, 2007;23(12):1320-1325.



