When sports chiropractors first appeared at the Olympic Games in the 1980s, it was alongside individual athletes who had experienced the benefits of chiropractic care in their training and recovery processes at home. Fast forward to Paris 2024, where chiropractic care was available in the polyclinic for all athletes, and the attitude has now evolved to recognize that “every athlete deserves access to sports chiropractic."
Flexion-Intolerant Lower Back Pain (Part 1): Diagnosis
Too often, we get fooled by pain. We forget that pain is a liar; we forget about sclerotomal referral. When the source of pain is the lower lumbar spine, the pain may be felt in the lumbar or sacroiliac area, buttock or down the leg.
As a practitioner, I appreciate the challenge of living in the gray zone. Spinal problems are so complex; so hard to wrap up in a simple package. Most low back pain has multiple contributing factors. I happen to love the mystery. My opinion is that the best chiropractors, the best physical therapists, the best interventional pain docs, the best surgeons, are the ones who keep their minds open.
I am not criticizing the goal of attempting to delineate subgroups. We have to do that to increase the percentage of patients we help, and to determine the right therapy for the individual patient. The success rate of many useful spinal treatments has been diluted by trying to apply them to every low back pain patient.
Flexion-Intolerant LBP
One large subgroup of our patients is best described by the term flexion-intolerant low back pain. This term was popularized by Stuart McGill, PhD. These patients primary have lower back pain, although they may have some referral into the buttock and/or down the leg, usually unilateral. They do not do well with sustained or repetitive flexion.
Do they have damage or irritation to a disc? I suspect most of them do. I also know this is a much more difficult diagnosis to definitely establish. The disc is deep in the body. The disc degenerates with age, so the number of false positives on imaging increases with age. The positive MRI, the bulged or herniated disc, is not a consistent guide to treatment.
Axial or low back pain coming from damaged discs has only recently been better understood. (This is not the time or place for a detailed description. If you would like to understand this better, read this thorough review article: "Clinical Diagnosis of Discogenic Low Back Pain."1) Quoting Zhang, "While the external outline of the disc may remain intact, multiple processes (degeneration, end plate injury, inflammation, etc.) can internally stimulate pain receptors inside the disc without nerve root symptoms."
The rehab researchers have contributed to a deeper understanding of what happens to the stabilizing musculature due to pain.2-4 Pain signals contribute to the vicious cycle. When pain signals come from the lower back, the deeper core muscles get inhibited or weak, and lose their ability to fire rapidly5 and anticipate movement.
Some of these muscles are small, and some practitioners and researchers discount them because of their size. But these muscles, including the multifidi and psoas, are optimally placed to provide translational stability. In Comerford's model,6 the function of what he calls the local stabilizers is not in a specific direction, but for stability, preventing uncontrolled movement. Remember that as we age, as the disc begins to shrink and the ligaments may get somewhat lax, so their stabilization function may be compromised.7
What about imaging? You might get lucky and see a high-intensity zone that tells you the patient has torn the disc. In obvious acute sciatic pain, the MRI may tell us the exact level and degree of disc herniation. But a high percentage of people have degeneration, disc bulges or even disc herniations on an MRI which may or may not create symptoms. To educate yourself further on imaging and on disc problems in general, I recommend a great site called www.chirogeek.com. Thanks for all your work on this, Dr. Gillard.

The dilemma is that we don't usually absolutely know whether the disc is causing the pain. What can we accurately assess? Can the patient tolerate flexion or not? This is relatively simpler and effectively guides our therapy.
These patients vary in how they present. Some will have an occasional severe episode of low back pain. Some will have chronic debilitating pain, and cannot stand or sit with comfort. The more symptomatic group is challenged by any sustained flexion, including sitting. Some of them will respond well to the conservative approach, especially if they are willing to do the work. Some may fail conservative care and need referral to medical specialists.
Let's discuss an approach, using the old-fashioned tools of history and physical exam, which can guide treatment for many of our acute and chronic lower back pain patients. This approach is potentially very cost-effective. It rarely requires advanced imaging. It often tells us quickly whether we are on the right track. It empowers the patient and gives them tools to manage their own back problems, both now and in the future. The exercise protocol can be simple for those who are only willing to do the basics; it can be sophisticated for those patients or athletes dedicated to optimizing their spinal function.
History Findings in Flexion Intolerance
What would make us suspect flexion-intolerant pain? Here are some of the history clues to consider:
- Does the patient have first-thing-in-the-morning pain or are they actually awakened by pain? This is usually a response to the swelling of the disc that occurs overnight.
- Do they have pain putting on their socks and shoes? This is usually an a.m. activity, when the disc is swollen, and involves prolonged flexion with a bit of rotation, the bane of the irritated disc.
- Do they have a history of a sudden shooting or sharp lower back pain? Did it occur from a lifting or bending injury? This is the usual way a disc injury occurs. Unless you ask the right questions, they may not remember how they were injured.
- Do they have a history of sciatica, or other buttock or leg pain? Obviously, they could have strained a knee or ankle, but leg pain should raise your suspicions. Some patients have a history of clear-cut discogenic sciatica, which they recovered from. In these cases, the disc was injured, and is likely to be more easily reinjured or reactivated.
- Do they have discomfort or pain getting in or out of a car or rolling over in bed? Rotation stresses the disc.
- Do they have discomfort or pain on getting up from sitting? Do they have pain from sitting, especially sitting in a non-supportive chair? Sitting is flexion. Prolonged sitting creates migration of the disc material posteriorly, irritating the sensitive annulus. Depending on how bad their problem is, a long sit may be 10 minutes or two hours. Getting up from sitting is often done poorly, with a flexion motion that loads the lumbar disc.
Physical Exam Findings
1. Observation findings: The trend we're looking for is a dysfunctional movement pattern, in which the patient does not control lumbar flexion. They do not hip hinge properly. They allow the lower lumbar spine to flex forward.
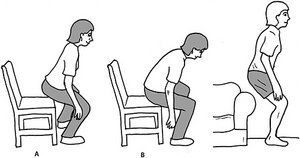
- Watch the patient get up from their seat in the waiting room. Do they maintain neutral or bend forward into flexion as they arise? Do they grimace with pain as they arise?
- In the treatment room, watch them take off their shoes.
- Toss a pen on the floor and ask them to pick it up.
- Look for fear or uncertainty at the prospect of bending forward.
2. Physical exam findings:
- Positive straight leg raise. Often you'll see more subtle findings than in classic sciatica. They may experience more tightness in the back of the leg on one side or the other. They may experience buttock pain. I prefer the sitting straight leg raise. If needed, add foot dorsiflexion, have the patient bend forward, and/or add a Valsalva maneuver.
- McGill quadruped rock back. Watch the patient who is on all fours rock back. Can they stay neutral? Have them do it slowly, and observe the point at which they lose the ability to stay neutral.
- One of Comerford's tests for flexion control is called the waiter's bow. Briefly teach the patient to bend forward while maintaining the spine in neutral. Stand to the side and watch them do this. Do they do it well or do they lose neutral? For tactile feedback, place your index finger horizontally on the sacrum, and the other hand's index finger just above, across the L5 spinous process. Now have the patient bend forward using the waiter's bow. Do your fingers separate? Recheck between L5 and L4. If your fingers are separating, the patient's lumbar spine in moving into flexion. It means that even when they are trying to, they cannot control flexion. See pictures below.
- Palpate the interspace for tenderness. Place the patient prone with a pillow under their abdomen, so the lumbar spine is in slight flexion. Apply deep digital pressure to the interspinous spaces and the inferior spinous process, pushing simultaneously posterior to anterior and inferior to superior. I start with L5-S1 and work upward to at least L3-4. Is the interspace tender? Ask them to rate the tenderness on a 1-3 scale: 1-mild, 2-moderate or 3-severe. (I used to think this was the ideal test, but it is not always positive, even in those I know have flexion intolerance. Maybe it represents increased inflammation in those with flexion intolerance.)
- Repeated end-range loading of extension (McKenzie-based). This can be done prone or standing. Does this relieve or centralize their pain?
- If they are not in acute pain, you can do repeated end-range loading of flexion, either from standing or in a long sit posture. Ask them to slump forward. Does this aggravate their pain; does this elicit increased buttock or leg pain, or sensory changes?
- Palpate the lower lumbar paraspinal muscles. In disc-related pain, a discrete area will often feel atrophied, often unilaterally. There is often a divot, a hole, a small area of atrophy, at the level of the disc injury. As chiropractors, we are much more used to getting information on the restricted side, rather than the side that is moving too much.
None of these tests is absolute. In some patients, the diagnostic impression is clear-cut. In others, you may need to put together multiple indicators to guide you. Sacroiliac misalignment and SI area pain are often found in flexion intolerance, and confuses many practitioners. A Craig Liebenson video serves as an excellent example of wading through the confusion.8
Treatment: An Introduction
Treatment of flexion-intolerant pain is primarily self-care. Yes, your soft-tissue work and mobilizations can help, but self-care is primary and essential. There is no magic you can do that will override what the patient is doing 24/7. You have to teach them to move differently to solve flexion-intolerant pain. According to Stuart McGill, "The first step in any exercise progression is to remove the cause of the pain, namely the perturbed motion and motor patterns."9
There are two components of self-care. First, have them quit doing stupid stuff that is reinjuring them over and over. Totally stop the sit-ups and crunches. They cannot do yoga-style prolonged flexion. Pilates is iffy, as it often uses too much uncontrolled flexion. Don't assume the patient knows this; they likely don't. If they are sitting too much and for too long, help them figure out how to change that habit via frequent breaks and/or by utilizing a standing workstation.
Second, train them to move differently. The exam findings lead directly into the basic self-care strategies. Teach them how to get up from sitting properly. Teach them to bend over standing, while maintaining lumbar neutral in the waiter's bow position. The hip hinge looks simple, but can be a challenge to learn. These movements fit in the category of teaching patients to quit hurting themselves.
Yes, they need to strengthen their inhibited core muscles, but they need start with these simple movements, done precisely. I send nearly all of my flexion-intolerant patients to www.fixyourownback.com. It's an excellent resource for patients with this type of back pain who are interested in taking care of themselves.
We have deliberately started the treatment description with self-care. We'll flesh out the appropriate exercise strategies in the next article. We'll also outline further in-office treatment, based on the joint-by-joint model, and discuss how to view manipulation and soft-tissue therapies through this lens.
References
- Yin-gang Zhang, Tuan-mao Guo, Xiong Guo, Shi-xun Wu. Clinical diagnosis for discogenic low back pain. Int J Biol Sci, 2009;5(7):647-658.
- Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode of low back pain. Spine, 1996;21(23):2763-2769.
- Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine, 1993;19(2):165-172.
- O'Sullivan P, Twomey L, Allison G, et al. Altered patterns of abdominal muscle activation in patients with chronic low back pain. Aust J Physio, 1997;43:91-98.
- MacDonald D, Moseley GL, Hodges PW. People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine, 2010 Apr 1;35(7):818-24.
- Gibbons SGT, Comerford MJ. Strength versus stability. Part 1: Concept and terms. Orthopaedic Division Review. March / April: 2001:21-27.
- Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine, 1994 Jun 15;19(12):1371-80.
- Liebenson C. "Flexion Intolerant Back" (10-minute video). Toronto, Ontario, 2011; filmed and edited by Phillip Snell.
- McGill S. "Designing Back Exercise: From Rehabilitation to Enhancing Performance." (Guide to training the flexion-intolerant back.)



