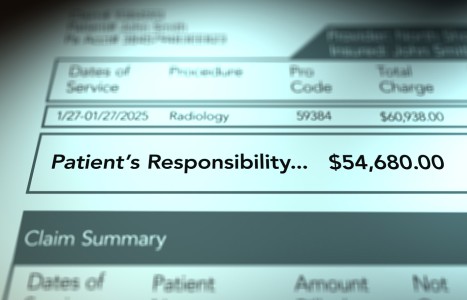
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Integrative Health Care for a Medicaid Population: Interview With Alan Post, DC
Editor's note: This interview appeared originally in the Nov / Dec 2012 issue of Health Insights Today, a newsletter published by Cleveland Chiropractic College – Kansas City. It is reprinted here with permission from the college.
Alan R. Post, DC, is past president of the Chiropractic Society of Rhode Island and the New England Chiropractic Council. He holds a Bachelor of Science in Human Biology and graduated with honors from Logan College of Chiropractic in 1982. At various points in his career, he has served as a state-appointed medical examiner for the Rhode Island Workers' Compensation System and as a member of the Rhode Island Blue Cross Specialty Advisory Board for Chiropractic and the Specialty Advisory Board for the Physician One Health Plan. He currently serves as a member of the advisory board at the University of Bridgeport Chiropractic College.
In this interview with Daniel Redwood, DC, Dr. Post describes the integrative medicine pilot program currently underway with Rhode Island Medicaid, which primarily serves low-income people in the state. In the preparatory stages of this Communities of Care project, he was a member of the Rhode Island Global Waiver Task Force, served on two committees that redesigned the state's Medicaid program, and also served on the Rhode Island Medicaid Stakeholder Committee.

Dr. Post has postgraduate certification in acupuncture and in 1993, traveled to China as a member of a North American physician delegation. Dr. Post has instructed physicians for continuing-education credentialing and is an integrative medicine program consultant. He is active in the current health care reform process, participating on a number of committees as both a member and a presenter. Dr. Post maintains two active patient care practices in Rhode Island and has received numerous awards for his professional service. In 2012, he contributed a chapter to the book Meditation as Medication for the Soul, by best-selling author Rajinder Singh.
We met recently at the premiere of the movie "Doctored." Afterward, we spoke about an integrative medicine pilot project in your home state, Rhode Island, where some Medicaid recipients are being placed in managed care programs that can include chiropractic care, acupuncture or massage therapy. This is modeled after an integrative care program implemented by Medicaid in Florida. Let me start by asking you: What specific problem or problems are there with Medicaid that projects such as this one seek to solve? In 2003, Alternative Medicine Integration (AMI)1-2 approached the Florida Health Care Administration and informed them that because of the lack of a specific diagnostic code or codes for chronic pain, they were not aware that chronic pain was one of the top three cost drivers in the Medicaid population. AMI had been able to analyze claims data through a proprietary program that works by keying into specific data elements. Included in these data elements are different diagnoses (again, because there's no ICD code for chronic pain).
But when you deal with a conglomeration of diagnoses including headaches, neck pain, back pain, fibromyalgia, chronic fatigue and some other neuromusculoskeletal conditions, what you find is that this is not only one of the largest cost drivers in the system, but [also] that the trendlines for people in this population increase far beyond the typical patient populations. Whereas the typical Medicaid trendline might increase by the standard related to health care inflation (between 6 and 10 percent per year), the chronic pain patient population rates can increase by almost 30 percent.
Are you talking about the percentage increase in costs? Yes, the trendline costs for managing care for the chronic pain patient population. With these patients the trendlining can be 30 percent. Also, in Rhode Island, the typical Medicaid patient today costs around $235 per member per month. The expenditures for the costliest chronic pain population, the "Communities of Care" population, are approximately $2,300 per patient per month. This group consists of patients who accessed the emergency room at least four times in a given year and have very high pharma costs. Their rate of increase is about 30 percent, so they're costing Medicaid 10 times the typical cost of regular enrollees.
In getting the Rhode Island pilot initiated, I set up a meeting with the director of Health and Human Services. He was informed about a problem that they had, which they didn't know they had. I was basing it on the data from the Florida program. Florida's was the first program in the country to get a waiver from CMS [Center for Medicare and Medicaid Services] for integrative medicine services to be paid for with federal tax dollars.
It was a breakthrough on many levels to accomplish that, and our profession should never let the importance of the political aspects of health care go unrecognized. We ignore these at our own peril and it will pose grave risk to ourselves into the future. The Florida program achieved savings of 18 percent.
When this integrative health care program was offered through Medicaid in Florida, you're saying that costs not only did not increase as much as usual, but they actually went down? They went down and they went down significantly. But that's only part of the good news. The other part was the outcome studies. SF evaluations [Short Form Health Evaluations such as SF-12 or SF-36] given at the beginning, before implementation of the programs, for both physical and mental components of function were then re-evaluated after the program. These demonstrated improvements of 16 to 22 percent upon re-evaluations.
A typical disease management program, if it's considered successful, will show an improvement in function of around 4 to 5 percent in the SF scores. The AMI integrative care population improved between 16 and 21 percent. That's a staggering number compared to traditional disease management interventions.
This is the kind of result that would really stand out and attract the attention of policy-makers, presumably. It did and it does. So, here we have reversal of cost trends, along with improved outcomes far beyond any traditional comparative stand-alone medical program. And then we have patient satisfaction surveys. The AMI program mailed out patient satisfaction surveys to their members, in a Medicaid population which, as you can imagine, was neither affluent nor highly educated. To elucidate further, the point-of-service information given to this population is written at a fourth-grade reading level, so you can understand that they're not very sophisticated.
Despite this, they had over a 35-percent return rate. Typically, on a mailer survey of this type, one is lucky to get a 5-percent, or if they're doing great, a 10-percent return rate, even in a typical population. Also, some of the patients' stories would literally bring tears to your eyes. There are patients who had significant transformative life experiences. Some of the satisfaction survey responses describe how their lives turned around and how it gave them hope.
One of the big parts of the success of the program is the empowering of the patient. These patients are disenfranchised socially and economically. Typically they are coming from home lives that are very distraught and dysfunctional. They have multiple comorbidities and they have issues with crime, violence, etc. They go into the medical system and, typically, they're treated like a faceless person, like a number. This can be unintentional. Unfortunately, it's the way many organizations and institutions tend to treat people, especially when they're doing it in high volume and at a low marginal return as experienced with a disenfranchised poor population such as this.
With the integrative care program, these people are coming in, they're being evaluated and then they are connected with a system of highly caring individuals, from the first contact with the holistic nurse case manager to the appropriate provider referral that is going to provide therapeutically appropriate pain interventions. The outcome you find is that they're reducing their medications and understanding that there are other ways of dealing with pain.
The patients are given point-of-service support materials on stress reduction, coping with conflict in the home, relaxation techniques and more. And they're receiving hands-on treatment. I trust that all our educational institutions are continually inspiring the soon-to-be new chiropractors, who are the future of our profession, with the importance and power found in the laying-on of hands and how important that component truly is. People's lives are being transformed.
So, this integrative medicine program has the potential to go well beyond providing effective pain treatment. What you're describing reflects the deep meaning of what the healing arts, at their best, are supposed to be about. Yes, it really does. RAND is now looking into integrative medicine's handling of chronic pain population and how it is that we can be so effective. This not just about saving money, though that is certainly in the forefront of people's awareness. It's also about the societal issues surrounding pharmaceutical pain medication: the potential for addiction, the dependency, the despondency created through the allopathic approach to pain management that all too often is not working well.
The system is basically broken. The leading cause of death in Rhode Island now is overdose from prescription medications. Fifty percent of emergency-room visits are now related to prescription medications. We have drug diversion issues with on-the-street crime and organized crime. This has become an epidemic. Here's an example: the leading pharmaceutical cost driver in the state of Vermont is Suboxone, which is a replacement of methadone.
Meaning it's an opioid. It supposedly reduces complications. What's happening with opioids is unbelievable. Recently in Florida, there have been many documented legal encounters between the doctors who run the "pill mills," the authorities and the licensing board. The stories of people who have flown down to Florida to get pain meds at these pill mills and then flown back with scripts, pills, and a business plan are well-documented in the press. This is a societal issue that has blown up and is out of control.
But it leads to a major opportunity for the integrative health care movement to move into a positive light on being able to deliver for those suffering from chronic pain. The road will not be easy as we seek to change the paradigm, because there are significant turf war issues going on and I foresee more emerging.
References
- Sarnat RL, Winterstein J. Clinical and cost outcomes of an integrative medicine IPA. J Manip Physiol Ther, June 2004;27(5):336-347.
- Sarnat RL, Winterstein J, Cambron JA. Clinical utilization and cost outcomes from an integrative medicine independent physician association: an additional 3-year update. J Manip Physiol Ther, May 2007;30(4):263-269.
Part 2 of this interview with Dr. Post is scheduled to run in the Sept. 1, 2013 issue of DC.