When sports chiropractors first appeared at the Olympic Games in the 1980s, it was alongside individual athletes who had experienced the benefits of chiropractic care in their training and recovery processes at home. Fast forward to Paris 2024, where chiropractic care was available in the polyclinic for all athletes, and the attitude has now evolved to recognize that “every athlete deserves access to sports chiropractic."
Enhancing Kinetic Chain Function to Treat Iliotibial Band Syndrome
Iliotibial band syndrome can be an ongoing source of pain and frustration for both practitioners and patients. Working with numerous professional and Olympic runners and cyclists, this is something I have seen frequently. The multitude of variables that can lead to an increase in stress and eventual injury of structures related to the iliotibial band further complicate the situation. Numerous structures influence the tension on the iliotibial track; if left unchecked, problems can lead to traction irritation of the distal attachment on the knee or frictional irritation over the lateral knee tubercle, causing pain.
One of the main contributing factors leading to iliotibial band syndrome is when there is too much adduction during gait due to overuse of adductors and weak hip abductors. This also increases the valgus stress on the knee during midstance, leading to torsional strain on the intra-articular components of the knee. The valgus strain on the knee during midstance increases the origin to insertion distance of the iliotibial track, which increases the insertional tension and friction created over the lateral tubercle.
Treatments for such conditions include articular adjustments, as well as localized soft-tissue work; not on the iliotibial track itself, but rather on the gluteus medius, vastus lateralis, biceps femoris and quadratus femoris, to name a few. Corrective strengthening exercises targeting motor control of the core with an emphasis on hip and ankle stability work quite well when dealing with chronic iliotibial band syndrome and similar cases.
Figure 1 and Figure 2 illustrate two examples of how to strengthen the hip abductors. The first exercise involves lying on the floor and performing a clam opening-like motion of the hip. This movement is performed with the spine maintained in a neutral position so hip motion can occur independent of the spine.
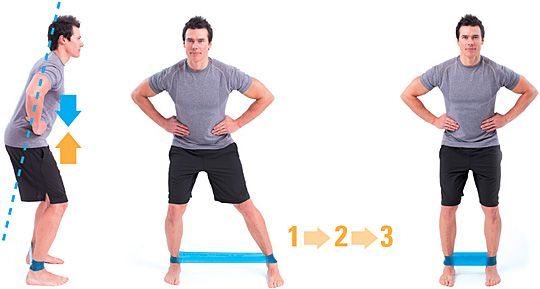
The progression for this motion is a lateral walk movement with a band attached around the ankles. The patient is instructed to step laterally while maintaining a neutral spine. I often tell patients to think about holding a glass of water on their head and not letting the glass tip over while stepping. I typically have them perform these movements, as well as others, for one set apiece every day of the week.

An often-missed, yet incredibly effective addition to the treatment plan for ITB syndrome and related conditions is taping. In fact, elastic therapeutic taping can make the difference in how quickly you are able to resolve such conditions due to the fact that your patients end up wearing their treatment in between your therapeutic sessions. By stimulating the touch receptors on the surface of the skin, the mechanical stimulation of the tape is converted into an electrical signal, which is then carried through the nervous system through a process called mechanotransduction.
There are a few different ways in which elastic therapeutic tape can help improve your clinical outcomes, dependent on how you apply the tape. I'm not talking about which direction you apply the tape; I'm talking about understanding the properties of the tape and determining what your clinical objectives are. Even with the advent of pre-cut and ready-to-apply applications, the clinical reasoning behind getting the best results is what matters.
For iliotibial band syndrome, the clinical goal is to identify the root cause of the condition so where you tape will have the greatest impact. Iliotibial band syndrome is a classic condition in that where your patients feel their discomfort is not necessarily where you need to be providing treatment. The abnormal mechanical stress and strain placed on the iliotibial band and knee due to the increased valgus strain must be corrected to effectively treat this condition.
Elastic therapeutic taping may be utilized in such a way as to provide the necessary afferent stimulation needed to encourage proper muscle activation, along with the prevention of potentially harmful ranges of motion. Both improper muscle activation (the hip abductors) and harmful movements (valgus stress at the knee) contribute to iliotibial band syndrome.

To illustrate treatment of this condition with taping, we need to examine the difference in applying a neurosensory technique versus a structural technique. Neurostructural technique is used when you principally wish to reduce the patient's level of discomfort while attempting to normalize motor activation in the muscles involved. Structural techniques are used when the main clinical goal is to reduce potentially harmful ranges of motion from occurring. A great example of a structural technique is applying elastic therapeutic tape across the back of the shoulders to improve posture and prevent forward rounding.
For taping the hip, I would first attempt to correct the imbalance by applying tape over the glut med or glut max directly while it is in a lengthened position, without any stretch being placed on the tape. You can determine the level of deficit, as well as how to gauge your impact of treatment, by employing dynamic movement evaluation strategies such as the squat test. You will clearly be able to see the leg deviating into valgus and can therefore use this to visualize the impact of taping.
If the initial taping strategy does not correct the imbalance and a valgus deviation is still present, I recommend two courses of action. One is to apply tape structurally to prevent internal rotation of the femur; the other is to initiate a targeted motor control exercise program. With either strategy I always, without exception, engage my patients in motor control rehabilitation. For the structural taping strategy, the body part is placed in a shortened position and you stretch the tape before applying it to the skin, so the tape becomes an external barrier that develops tension. This prevents the end ranges of motion you are trying to avoid. Figure 4 demonstrates how to tape the lateral leg from the hip with the tape being stretched before it is applied on shortened tissue.
Try including these strategies as a part of your treatment plan for patients with iliotibial band syndrome, and let me know how it goes. I am always interested in hearing about your results.



