In a landmark development, Blue Cross Blue Shield (BCBS) has reached a $2.8 billion settlement to resolve antitrust claims brought by health care providers, including chiropractors. The lawsuit accused BCBS of dividing the nation into exclusive regions and limiting competition, which resulted in lower reimbursements for providers. Although BCBS denies any wrongdoing, the company agreed to the settlement to avoid lengthy litigation – and you can get a piece of the pie.
Posttraumatic Osteolysis of the Clavicle
Patients commonly present to the chiropractic office with shoulder complaints. Several conditions may be responsible. One such entity is posttraumatic osteolysis of the clavicle (PTOC). It is important for the clinician to recognize this not-so-common condition, both clinically and radiographically, and to have it available as a differential diagnosis. If a patient meets the diagnostic criteria and there is a delay in patient response to treatment, this condition should be considered. The purpose of this article is to inform the chiropractor about PTOC.
The Condition
Distal osteolysis of the clavicle associated with trauma was first described in 1936.1,2 Initially believed to be a sequelae of acromioclavicular joint separation, it is now also recognized as being associated with minor shoulder trauma and strenuous exercise.1 Many reports now exist of PTOC occurring as a result of strenuous physical exercise involving the upper extremities, including weightlifting, handball and baseball.1-3 Posttraumatic osteolysis is not only seen in the distal clavicle, but also can occur at the medial clavicle, pubic symphysis and ischial rami, distal ulna and radius, carpal bones, distal phalanges, and the femoral neck.1,2 The exact cause of the osteolysis is still unknown and subject to debate; hypotheses include avascular necrosis, autonomic dysfunction, synovial hyperplasia and hyperemia.1-3 If untreated, the osteolysis may extend up to 3 centimeters into the bony substance of the distal clavicle over a period of 12-18 months.2,3 The condition is self-limiting; with the appropriate management, reparative changes can be seen within four to six months. Final outcomes vary from complete restoration of the clavicle to a tapered, irregular appearance.2,3
The Patient
PTOC typically affects males in their late teens to early 40s.1 The patient is generally very active and develops shoulder pain following trauma or continued strenuous physical activity involving the upper extremity. Patients who present with PTOC following acute trauma typically experience unilateral shoulder pain weeks to months after the trauma.1,3 The pain is generally mild to moderate. Pinpoint pain at the acromioclavicular joint is common and can be associated with a lump or swelling.1 Shoulder range of motion can be full, but also can be reduced due to pain.1-3 Patients with PTOC who have not had acute trauma will most likely present with a history of strenuous physical activity and a gradual onset of pain, but the remaining clinical picture will be almost identical to the acute onset following trauma. However, one important difference is that both shoulders typically are involved in this scenario.1,2 Because this onset is found in those who engage in more intense physical activity, and because it is especially common in weightlifters,2,3 the pain may be ignored early on as the patient typically continues to exercise through the pain. They will, however, reach a point at which the pain becomes too intense to continue the activity at their expected level of intensity. Some patients complain that the pain will persist days after the activity.1
Imaging
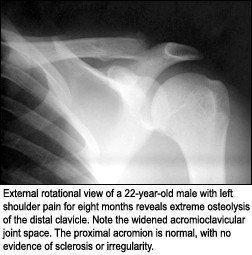
It is imperative that high-quality radiographs are generated, as the imaging findings can be subtle and may be missed on substandard radiographs. The initial radiographic findings include a loss of bone density and loss of subarticular bone at the distal clavicule.1,2 The condition typically progresses to a more lytic phase, in which there will be erosive lucencies at the subchondral region of the distal clavicle. The typical degree of osteolysis is approximately 1-3 millimeters into the bony substance of the distal clavicle within three months from the time of injury.1-3 The findings can be more extreme with complete erosion or absence of the distal portion of the clavicle. The osteolysis can be identified on the radiographs within two to three months following the acute injury.1-3 When initiated by chronic stress, it can be visible on the radiographs as early as two to three weeks.1,2 It may present as widening of the acromioclavicular joint, with either subtle erosion or complete osteolysis of the clavicle. The normal measurement at the acromioclavicular joint should range from 2.5 to 4 millimeters.2,3
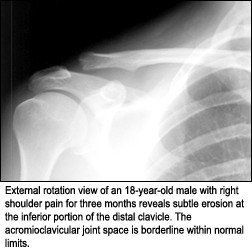
To better visualize the AC joint on an AP projection, a 13° to 35° cephalad tube tilt can be used; views of the opposite shoulder offer a baseline for comparison in subtle cases.1 Once healing begins, there can be complete repair of the clavicle resulting in a normal radiographic appearance, or there may be partial deformity with a widened AC joint. Again, this will occur over a period of four to six months.1-3 In cases in which a diagnosis must be made and there are no radiographic findings to substantiate one, advanced imaging can be ordered to confirm a diagnosis. Bone scans will demonstrate increased uptake, and magnetic resonance imaging will demonstrate a high signal on T2-weighted sequences at the distal clavicle.1 The differential diagnosis for the radiographic appearance of osteolysis at the distal clavicle would include hyperparathyroidism, collagen vascular disorders, infection and rheumatoid arthritis.2
Treatment
Initial management of this condition is primarily conservative and consists of ice, sling immobilization, analgesics, and elimination of provocative activities.1 This may not prevent continued osteolysis or shorten the time for bony restoration,1-3 but early treatment may reduce the total amount of bone loss and degree of clinical symptoms. If the patient is not responding as anticipated, corticosteroids can be used. However, success with corticosteroids has been limited and the patient may continue to experience pain.1 In extreme cases in which there is persistent pain and no response to conservative management, surgical resection of the distal clavicle may be considered.1
Summary
Posttraumatic osteolysis of the clavicle is an uncommon condition that must not be overlooked in our active patients with shoulder pain. A thorough history and quality radiographs should be enough to make the diagnosis, but in instances in which there are no radiographic findings, repeat studies or advanced imaging may be necessary for an accurate diagnosis. Conservative treatment is often enough to properly manage this condition; however, in rare instances, extreme measures such as resection of the distal clavicle may be necessary.
References
- Mestan M, Bassano J. Posttraumatic osteolysis of the distal clavicle: analysis of 7 cases and a review of the literature. JMPT 2001;24(5):356-361.
- Resnick, D, Niwayama, G. Diagnosis of Bone and Joint Disorders, 3rd ed. Philadelphia: W.B. Saunders, 1995.
- Yochum T, Rowe L. Essentials of Skeletal Radiology, 3rd ed. Baltimore: Williams & Wilkins, 2005.



