When sports chiropractors first appeared at the Olympic Games in the 1980s, it was alongside individual athletes who had experienced the benefits of chiropractic care in their training and recovery processes at home. Fast forward to Paris 2024, where chiropractic care was available in the polyclinic for all athletes, and the attitude has now evolved to recognize that “every athlete deserves access to sports chiropractic."
Diagnosing Anterior Cruciate Ligament Tear
I'm not a great skier, but I love to be on a snow-covered mountain and to experience winter and all its beauty. One of the more common ski injuries involves the knees, and it usually occurs when people try to ski and train above their abilities. Boots and bindings are so good now that the knees bear the brunt of falls. (Head injuries are also common, but some skiers are now wearing helmets.)
Of the injuries that occur in the knee, the anterior cruciate ligament is most commonly injured. A tear in this ligament usually occurs following a sudden valgus impact, accompanied by pain and swelling. On careful physical examination, experienced clinicians may be able to obtain most of the information required to make the diagnosis of an anterior cruciated injury. However, even an experienced examiner may have difficulty assessing the extent of the injury. A patient's pain and muscular spasm may prevent adequate examination.
There are several orthopedic tests evaluating an anterior cruciated injury, but Lachman's test is touted as the most specific and reliable, as far as orthopedic tests go. I generally prefer to examine the knee with an MRI study, since I can generally see the extent of the injury and determine how aggressive the treatment need be.
Injury to a cruciate ligament may not always cause pain. Rather, the person may hear a popping sound, and the leg may buckle when the person tries to stand. An MRI is very accurate in detecting a complete tear (97 percent accurate), but arthroscopy may be the only reliable means of detecting a partial tear.

Figure 1: LachmanÍs test of the right knee. The examiner used the right hand to place anterior force on the lower leg while simultaneously using the left hand to place posterior force on the distal thigh. A good end point should be felt. Hands are reversed to test the left knee.
For an incomplete tear, the patient may respond to conservative treatment that should include an exercise program to strengthen surrounding muscles. A protective knee brace may also help patients during activity. For a completely torn anterior cruciate ligament in an active athlete and motivated patient, surgery is generally recommended. The surgeon may reattach the torn ends of the ligament, or reconstruct the torn ligament by using a grafted ligament from the patient (autograft), or from a cadaver (allograft). Although repair using synthetic ligaments has been tried experimentally, the procedure has not yielded better results than use of human tissue.

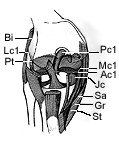

Figure 2: Anterior cruciate avulsion. The anterior cruciate has been avulsed from its femoral avulsion and lies inferiorly on the tibial plateau (arrows).
One of the most important elements in a patient's successful recovery after cruciate ligament surgery is following an exercise and rehabilitation program for four to six months. Successful surgery and rehabilitation will allow the patient to return to a normal full lifestyle.


Distal anterior cruciate avulsion. On the left, a normal anterior cruciate is seen. The anterior band is shown by the straight arrow, the posterior band by the curved arrow. On the right, the proton image (above) and the T2 weighted (below) images show partially attenuated anterior cruciate ligaments, partly torn from their distal insertions. Far right 2mm thick 3DFT image from a different patient shows avulsion at the distal insertion (curved arrow).
References
- Andrews M, Noyes F, et al. Anterior cruciate ligament allograft reconstruction in the skeletally immature athlete. Am J Sports Med, Vol. 22, No.1, pp. 48-54. 1994.
- Bertin K, et al. Ligament injuries associated with physeal fractures about the knee. CORR, No. 177, pp. 188-195. July/ August 1983.
- Clanton T, DeLee J, et al. Knee ligament injuries in children. JBJS, 61-A, No. 8, pp. 1195-1201. December 1979.
- DeLee J, et al. Anterior cruciate ligament insufficiency in children. CORR, No. 172, pp. 112-8. Jan/Feb 1983.
- Engebretsen L, et al. Poor results of anterior cruciate ligament repair in adolescence. Acta Orthop Scand 1988; 59(6): pp. 684-6.
- Kannus P, et al. Knee ligament injuries in children. JBJS, 70-B, No. 5, pp. 772-6. November 1988.
- Lipscomb B, Anderson A, et al. Tears of the anterior cruciate ligament in adolescents. JBJS, 68-A, No. 1. pp. 19-28. Jan 1986.
- McCarroll J, Shelbourne K, et al. Anterior cruciate ligament injuries in the young athlete with open physes. Am J Sports Med, Vol. 16, No. 1, pp. 44-47. 1988.
- Parker A, Drez D, et al. Anterior cruciate ligament injuries in patients with open physes. Am J Sports Med, Vol. 22, No. 1, pp. 44-47. 1994.
- Polly D, et al. The accuracy of selective MRI compared with the findings of arthroscopy of the knee. JBJS, 70-A, No. 2, pp. 192-8. Feb 1988.
- Munk P, Helms C. MRI of the Knee. Aspen Publications pp. 25-31, 1992
Deborah Pate,DC,DACBR
San Diego, California
patedacbr@cox.net



